-
Volume 71,
Issue 6,
2022
-
Volume 71,
Issue 6,
2022
Volume 71, Issue 6, 2022
- Reviews
-
-
-
Disinfection methods of dental unit waterlines contamination: a systematic review
More LessBackground. Severe contamination of dental unit waterlines was found in healthcare settings. The benefits of decontamination methods are controversial. The aim of this review was to systematically evaluate disinfection methods in contamination control of dental unit waterlines.
Methods. The terms ‘dental unit waterline(s) or DUWL(s) or dental unit water line(s)’ were searched through PubMed, Cochrane Library, Embase, Web of Science and Scopusup to 31 May 2021. The DUWLs’ output water was incubated on R2A agar at 20–28 °C for 5–7 days to evaluate heterotrophic mesophilic bacteria. The risk of bias was evaluated by a modified Newcastle-Ottawa quality assessment scale.
Results. Eighteen papers from the literature were included. One study indicated that water supply played a crucial role in disinfecting DUWLs. Three studies indicated that flushing decreased bacteria counts but did not meet the American CDC standard (500 c.f.u. ml−1). All chlorine- and peroxide-containing disinfectants except sodium hypochlorite in one of 15 studies as well as three mouthrinses and citrus botanical extract achieved the standard (≤500 c.f.u. ml−1). The included studies were of low (1/18), moderate (6/18) and high (11/18) quality.
Conclusion. Independent water reservoirs are recommended for disinfecting DUWLs using distilled water. Flushing DUWLs should be combined with disinfections. Nearly all the chlorine-, chlorhexidine- and peroxide-containing disinfectants, mouthrinses and citrus botanical extract meet the standard for disinfecting DUWLs. Alkaline peroxide would lead to tube blockage in the DUWLs. Regularly changing disinfectants can reduce the risk of occurrence of disinfectant-resistant strains of microbes.
-
-
-
-
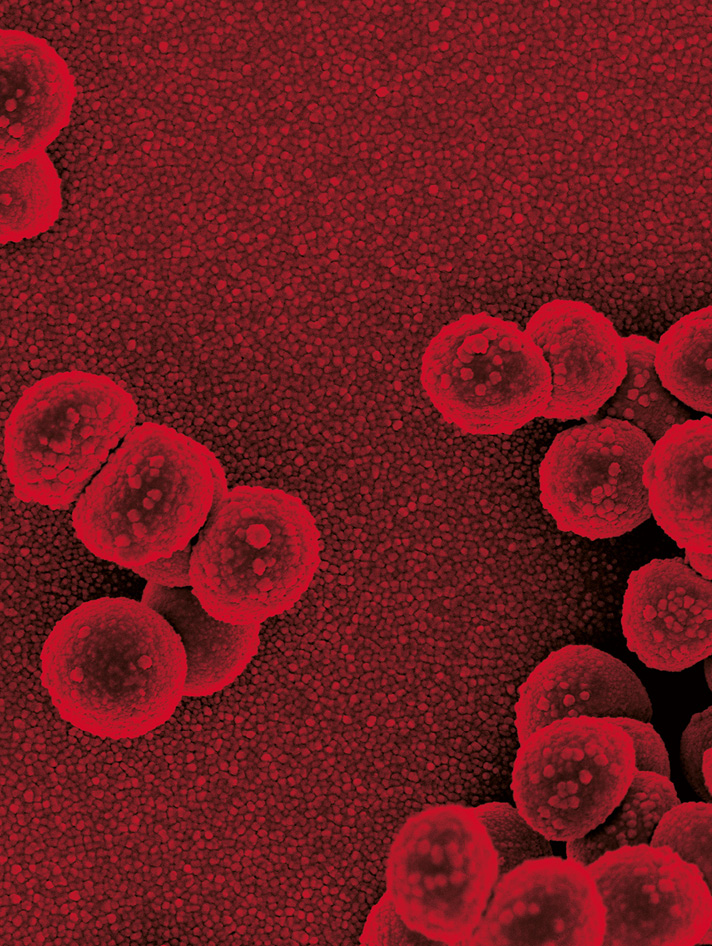
Emerging strategies for environmental decontamination of the nosocomial fungal pathogen Candida auris
More LessCandida auris is a recently emerged multidrug-resistant fungal pathogen that causes life-threatening infections to the human population worldwide. Recent rampant outbreaks of C. auris in coronavirus disease 2019 (COVID-19) patients, together with outbreaks in over 45 countries, highlight its threat to patients and healthcare economies. Unlike other pathogenic Candida species, C. auris is capable of surviving in abiotic surfaces of healthcare facilities for prolonged periods, leading to increased risk of transmission within nosocomial settings. C. auris is resistant to multiple classes of antifungal agents, forms dry biofilms and transmits independently to regional epicentres, making its eradication from nosocomial environment arduous. The lack of strategies for environmental decontamination of C. auris from nosocomial settings is evident from the generic guidance and recommendations provided by leading global healthcare bodies. Therefore, this minireview discusses the current guidelines for environmental decontamination of C. auris and compounds and strategies currently under investigation for potential future use. While established guidelines recommend the use of products mainly consisting of sodium hypochlorite and hydrogen peroxide, initial works have been reported on the promising anti-C. auris properties of various other compounds and some biocompatible alternatives. Further validation of these approaches, coupled up with environmentally friendly decontamination protocols, are warranted to achieve superior elimination of C. auris from healthcare settings.
-
- Antimicrobial Resistance
-
-
-
Genetic characteristics of azithromycin-resistant Neisseria gonorrhoeae collected in Hyogo, Japan during 2015–2019
More LessIntroduction. Azithromycin (AZM) is a therapeutic drug for sexually transmitted infections and is used for Neisseria gonorrhoeae when first- and second-line drugs are not available. Recently, the susceptibility of N. gonorrhoeae against AZM has been decreasing worldwide.
Hypothesis/Gap Statement. Azithromycin-resistance (AZM-R) rates among N. gonorrhoeae in Japan are increasing, and the gene mutations and epidemiological characteristics of AZM-R in N. gonorrhoeae have not been fully investigated.
Aim. We determined the susceptibility to AZM and its correlation with genetic characteristics of N. gonorrhoeae .
Methodology. We investigated the susceptibility to AZM and genetic characteristics of N. gonorrhoeae . Mutations in domain V of the 23S rRNA gene and mtrR were examined in 93 isolates, including 13 AZM-R isolates. Spread and clonality were examined using sequence types (STs) of multi-antigen sequence typing for N. gonorrhoeae (NG-MAST), and whole genome analysis (WGA) to identify single nucleotide polymorphisms.
Results. The number of AZM-R isolates increased gradually from 2015 to 2019 in Hyogo (P=0.008). C2599T mutations in 23S rRNA significantly increased in AZM-R isolates (P<0.001). NG-MAST ST4207 and ST6762 were frequently detected in AZM-R isolates, and they had higher MICs to AZM from 6 to 24 µg/ml. The phylogenic tree-based WGA showed that all isolates with ST4207 were contained in the same clade, and isolates with ST6762 were divided into two clades, AZM-S isolates and AZM-R isolates, which were different from the cluster containing ST1407.
Conclusion. Our study showed yearly increases in AZM-R rates in N. gonorrhoeae . NG-MAST ST4207 and ST6762 were not detected in our previous study in 2015 and were frequently identified in isolates with higher MICs to AZM. WGA confirmed that isolates with these STs are closely related to each other. Continued surveillance is needed to detect the emergence and confirm the spread of NG-MAST ST4207 and ST6762.
-
-
-
-
Antifungal activity and potential mechanism of berberine hydrochloride against fluconazole-resistant Candida albicans
More LessIntroduction. The emergence of resistance to fluconazole in Candida albicans has made the clinical treatment of this microbe difficult. A potential strategy to address this problem involves diminishing fungal resistance to antimicrobial drugs.
Hypothesis. Berberine hydrochloride (BH), the primary active ingredient of the traditional Chinese medicine (TCM) Coptis, inhibits the growth of fluconazole-resistant C. albicans through its action on the high-osmolarity glycerol mitogen-activated protein kinase (HOG-MAPK) pathway.
Aim. To examine the effect of BH on the HOG-MAPK pathway to assess the potential molecular mechanism by which BH inhibits fluconazole-resistant C. albicans.
Methodology. The minimum inhibitory concentration (MIC) of BH to fluconazole-resistant C. albicans was measured using the broth microdilution approach to determine the concentration of effective drug intervention. Changes in physiological functions regulated by the HOG-MAPK pathway in response to BH treatment were measured, as well as the expression of central signalling pathway genes and key downstream factors by qRT-PCR and Western blotting, respectively.
Results. BH inhibited fluconazole-resistant C. albicans and the sensitivity to fluconazole increased after BH treatment. At a concentration of 256 and 64 μg ml−1 BH may affect key downstream factors that regulate several physiological functions of C. albicans by upregulating the core genes expression of SLN1, SSK2, HOG1, and PBS2 in the HOG-MAPK pathway. Upregulation of GPD1, the key gene for glycerol synthesis, increased cell osmotic pressure. BH treatment increased the accumulation of reactive oxygen species by upregulating the expression of the key respiratory metabolism gene ATP11 and downregulating the expression of the superoxide dismutase gene SOD2. Furthermore, downregulation of mycelial-specific HWP1 hindered the morphological transformation of C. albicans and inhibition of the chitin synthase gene CHS3 and the β-(1,3) glucan synthase gene GSC1 impaired cytoderm integrity.
Conclusion. BH affects multiple target genes in diminishing the resistance of C. albicans strains to fluconazole. This effect may be related to the action of BH on the HOG-MAPK pathway.
-
-
-
RshA mutations contributing to tigecycline resistance in Mycobacteroides abscessus
More LessTigecycline is an important rescue antibiotic for many bacterial infections. In Mycobacteroides abscessus , tigecycline resistance has been associated with dysregulated stress response caused by aberrations in the interaction of the SigH and RshA factors. In this study, two tigecycline-resistant mutants of M. abscessus (CL5A and CL6A) with mutations in the rshA gene were studied using gene complementation, RT-qPCR and the bacterial adenylate cyclase two-hybrid (BACTH) system. The results supported the premise that mutations in the rshA interrupt the RshA–SigH interaction to cause the overexpression of the sigH gene that leads to tigecycline resistance or reduced susceptibility.
-
-
-
In vitro activity of fidaxomicin against nontuberculosis mycobacteria
More LessIntroduction. Nontuberculous mycobacteria (NTM) infections are increasing worldwide and are relatively resistant to many of the first- and second-line drugs to treat tuberculosis. Macrolide antibiotics, such as clarithromycin and azithromycin, are the key drugs for treating NTM infections. Fidaxomicin is a macrolide antibiotic that is widely used in treating Clostridium difficle (C.difficile) infections, and has high in vitro activity against Mycobacterium tuberculosis especially multidrug-resistant tuberculosis (MDR-TB) and has no cross-resistance with rifampicin.
Hypothesis. Fidaxomicin may have in vitro activity against NTM strains.
Aim. To find that whether the macrolide antibiotic fidaxomicin has in vitro activity against NTM strains.
Methodology. Fidaxomicin used in this study was firstly tested on C. difficile reference strains and has shown to be effective and workable. And then 28 rapidly growing mycobacteria (RGM), 12 slowly growing mycobacteria (SGM) reference strains and 103 NTM clinical isolates were tested by the microplate-based AlamarBlue assay (MABA) method to determine the MICs. Fidaxomicin, rifampicin and clarithromycin were tested against M. abcessus complex subspecies 14 M . abscessus and 5 M . massiliense strains for inducible resistance determination.
Results. In total, 21 out of 28 RGM and 9 of 12 SGM reference strains have the MICs of fidaxomicin at or below 1 µg ml−1. Fidaxomicin also showed low MIC values for some clinical isolates including M. abscessus complex, M. avium complex, M. fortuitum , M. kansasii and M. parascrofulaceum . Fidaxomicin also has no inducible macrolide resistance in M. abscessus complex in comparison with clarithromycin.
Conclusion. Fidaxomicin has high in vitro activity against most of the NTM reference strains and some prevalent NTM clinical isolates. This promising finding warrants further investigation on the actions of fidaxomicn in vivo and as a potential antibiotic for NTM treatment.
-
-
-
Aminoglycoside resistance in Pseudomonas aeruginosa: the contribution of the MexXY-OprM efflux pump varies between isolates
More LessIntroduction. Aminoglycoside antibiotics are widely used to treat infections of Pseudomonas aeruginosa . The MexXY-OprM efflux pump is an important contributor to aminoglycoside tolerance in P. aeruginosa reference strains and expression of the mexXY genes is repressed by the MexZ repressor protein. Direct investigation of the role of this efflux pump in clinical isolates is relatively limited.
Hypothesis. The contribution of MexXY-OprM to P. aeruginosa aminoglycoside resistance is isolate-specific.
Aim. To quantify the role of MexXY-OprM and its repressor, MexZ, in clinical isolates of P. aeruginosa.
Methodology. The mexXY genes were deleted from ten clinical isolates of P. aeruginosa , and the mexZ gene from nine isolates. Antimicrobial susceptibility testing was carried out for commonly used antipseudomonal drugs on the engineered mutants and the isogenic wild-type isolates. RT-qPCR was used to measure expression of the mexX gene.
Results. All but one of the mexXY mutants were more susceptible to the clinically used aminoglycosides tobramycin, gentamicin and amikacin but the degree to which susceptibility increased varied greatly between isolates. The mexXY mutants were also more susceptible to a fluoroquinolone, ciprofloxacin. In three isolates with functional MexZ, deletion of mexZ increased expression of mexXY and aminoglycoside tolerance. Conversely, deleting mexZ from six clinical isolates with mexZ sequence variants had little or no effect on expression of mexXY or on aminoglycoside susceptibility, consistent with the variants abolishing MexZ function. Genome analysis showed that over 50 % of 619 clinical isolates had sequence variants predicted to reduce the affinity of MexZ for DNA, likely increasing mexXY expression and hence efflux of aminoglycosides.
Conclusion. Our findings show that the interplay between MexXY, MexZ and the level of mexXY expression plays an important role in aminoglycoside resistance in clinical isolates of P. aeruginosa but the magnitude of the contribution of this efflux pump to resistance is isolate-specific.
-
-
-
Evaluation of NG-Test CARBA 5 for the detection of carbapenemase-producing Gram-negative bacilli
More LessCarbapenemase-producing Enterobacterales (CPE) pose one of the most serious antimicrobial resistance threats to public health worldwide. The outcome of CPE infection differs depending on the resistance mechanism. Therefore, rapid detection of CPE infection is essential for optimizing patient management. The carbapenem inactivation method (CIM) and modified CIM (mCIM) are standard methods for detecting CPE, but they usually require 24 h to generate results.
Recently, an immunochromatographic assay, NG-Test CARBA 5, has become commercially available. It detects the five most common carbapenemase producers (KPC, IMP, NDM, VIM, and OXA-48) rapidly and accurately.
We aimed to evaluate the diagnostic accuracy of NG-Test CARBA 5 for detecting carbapenemase-producing Gram-negative bacilli (CPGNB).
We used 116 carbapenemase-producing strains and 48 non-carbapenemase-producing strains. Of the 116 carbapenemase-producing strains, 107 harboured genes for at least one of the five most common carbapenemases, KPC, IMP, NDM, VIM, and OXA-48-like. Forty-eight non-carbapenemase-producing strains, including carbapenem-resistant Enterobacterales , harboured genes for extended-spectrum β-lactamases (CTX-M groups [n=25] and SHV groups [n=2]) or plasmid-mediated AmpC β-lactamases (DHA [n=3], CMY-2 [n=2], and CFE-1 [n=1]). Antimicrobial susceptibility was tested using the agar dilution method, according to the Clinical and Laboratory Standards Institute guidelines.
Of the 116 carbapenemase-producing strains, 79 were resistant to at least meropenem or imipenem. The sensitivity and specificity of the NG-Test CARBA 5 for the strains were 99.1 % (106 strains positive for 107 strains of the five most common carbapenemase producers) and 100 % (60 strains negative for other types of CPGNB [n=10] and non-CPGNB strains [n=48]), respectively. The carbapenemase-producing strain with a false-negative result produced IMP-66.
The NG-Test CARBA 5 had high sensitivity and specificity for detecting carbapenemase-producing strains.
-
- Clinical Microbiology
-
-
-
Clinical characteristics and antimicrobial susceptibility of Klebsiella pneumoniae, Klebsiella variicola and Klebsiella quasipneumoniae isolated from human urine in Japan
More LessIntroduction. The three Klebsiella species K. pneumoniae , K. variicola and K. quasipneumoniae are difficult to distinguish, owing to their similar biochemical properties, and are often confused in medical practice.
Gap statement. There is a scarcity of data comparing the clinical characteristics and antimicrobial susceptibility of K. pneumoniae , K. variicola and K. quasipneumoniae . We believe that knowledge of the characteristics of each species will help in their better identification. Further, knowing the antimicrobial susceptibility of the species will help physicians in prescribing an effective treatment course for Klebsiella infections.
Aim. This study aimed to determine the clinical characteristics and antimicrobial resistance of K. pneumoniae , K. variicola and K. quasipneumoniae isolated from human urine samples.
Methodology. This study included 125 K . pneumoniae strains isolated from human urine samples. Multiplex polymerase chain reaction was performed to identify K. pneumoniae , K. variicola and K. quasipneumoniae . We retrospectively investigated the patient background, complications of bacteraemia, antimicrobial susceptibility and extended-spectrum β-lactamase (ESBL).
Results. We identified 84 (67.2 %), 31 (24.8 %) and 10 strains (8 .0%) of K. pneumoniae , K. variicola and K. quasipneumoniae , respectively. There was no difference in patient background and frequency of bacteraemia complications among these species. K. pneumoniae was significantly less susceptible than K. variicola to ampicillin/sulbactam (P=0.03) and piperacillin (P<0.01). Furthermore, K. pneumoniae (79.8 %) was less susceptible to trimethoprim/sulfamethoxazole than K. variicola (96.8 %) and K. quasipneumoniae (100 %). There were nine ESBL-producing strains (7.2 %), all of which were K. pneumoniae .
Conclusion. There was no difference in patient background and frequency of bacteraemia complications between K. pneumoniae , K. variicola and K. quasipneumoniae isolated from urine. The three Klebsiella species showed a varying extent of antimicrobial susceptibility and ESBL production, and accurate identification is needed to understand the epidemiology of these species.
-
-
-
-
Isolation of Clostridioides difficile PCR Ribotype 027 from single-use hospital gown ties
More LessBackground. Clostridioides difficile is a spore-forming pathogen responsible for antibiotic-associated diarrhoea. In the USA high incidence of C. difficile infection (CDI) in clinical environments has led to interest in C. difficile spore transmission.
Hypothesis. Single use hospital surgical gown ties act as a reservoir for C. difficile spores.
Aim. This study sought to examine whether single-use hospital surgical gown ties used in surgery, from an acute healthcare facility, harboured C. difficile spores.
Methodology. Used surgical gowns ties worn by clinicians in the healthcare facility were examined for C. difficile spore presence via spread plate and anaerobic culture. The colonies isolated from each gown tie were subcultured on C. difficile selective agar for phenotypic confirmation. Presumptive C. difficile colonies were examined using C. difficile Quik Check Complete, 16–23S PCR Ribotyping and MALDI-TOF analysis.
Results. In total 17 suspected C. difficile colonies were isolated from 15 gown ties via culture. C. difficile Quik Check Complete found two isolates as possible C. difficile . MALDI-TOF and PCR Ribotyping confirmed one isolate as C. difficile PCR ribotype 027 associated with clinical outbreaks.
Discussion. Our study revealed the presence of hypervirulent C. difficile ribotype 027 spores on single-use gown ties. This highlights the potential of gown ties as a vector of spore transmission across clinical environments, especially when gowns are not worn appropriately.
Conclusions. Appropriate compliance to infection control procedures by healthcare workers is essential to prevent spore dissemination across clinical facilities and reduce CDI rates.
-
- Disease, Diagnosis and Diagnostics
-
-
-
The impact of VITEK 2 implementation for identification and susceptibility testing of microbial isolates in a Brazilian public hospital
More LessIntroduction. The use of automated systems in identification and susceptibility tests can improve antimicrobial therapy, and positively impact clinical outcomes with a decrease in antimicrobial resistance, hospitalization time, costs, and mortality.
Aim. The aim of this study was to evaluate the clinical impact of an automated method for identification and susceptibility testing of microbial isolates.
Methodology. This was a retrospective cross-sectional study aimed to analyse the results before and after the implementation period of a VITEK 2 system in a Brazilian university hospital. Based on data from medical records, patients with a positive culture of clinical samples from January to July 2017 (conventional method) and from August to December 2017 (automated method) were included in this study. Demographic data, hospitalization time, time interval between culture collection and results, culture results and site, susceptibility profile, minimum inhibitory concentration, and outcome data were evaluated. Chi-square and Fischer’s tests were used in the analysis.
Results. Of the total samples, 836 were considered valid by the inclusion criteria, with 219 patients before VITEK 2 system implementation group and 545 in the post-implementation group. The comparison between the two periods showed a reduction of 25 % of the time to culture reports, a decrease of 33.5 to 17.0 days of hospitalization, and a reduction in mortality from 44.3–31.0 %, respectively.
Conclusion. The VITEK 2 system provided early access to appropriate antimicrobial therapy for patients and effected a positive clinical impact with a reduction in mortality and hospitalization time.
-
-
-
-
Combined oropharyngeal/nares and nasopharyngeal swab sampling remain effective for molecular detection of SARS-CoV-2 Omicron variant
More LessThe world has experienced several waves of SARS-CoV-2 variants of concern (VoCs) throughout the COVID-19 pandemic since the first cases in December 2019. The Omicron VoC has increased transmission, compared to its predecessors, and can present with sore throat and other cold-like symptoms. Given the predominance of throat symptoms, and previous work demonstrating better sensitivity using antigen-based rapid detection tests when a throat swab is included in the standard nasal sampling, this quality improvement project sought to ensure ongoing suitability of both combined oropharyngeal/nares (OPN) and nasopharyngeal (NP) swab sampling used throughout the pandemic. Consenting participants meeting Public Health testing criteria (mostly symptomatic or a close contact of a known case) were enrolled, and paired NP and OPN swabs were subjected to nucleic acid amplification testing (NAAT). Comparing paired specimens from 392 participants sensitivity of NP swabs was 89.1 % (95 % CI, 78.8–94.9), and that of OPN was 98.4 % (95 % CI: 90.9->99.9) (P-value 0.052). This project demonstrated that both NP and combined OPN swabs detected the Omicron variant with similar sensitivity by NAAT, supporting the continued use of either swab collection for SARS-CoV-2 molecular detection.
-
-
-
Volatile compounds from in vitro metabolism of seven Listeria monocytogenes isolates belonging to different clonal complexes
More LessMicroorganisms produce a wide variety of volatile organic compounds (VOCs) as products of their metabolism and some of them can be specific VOCs linked to the microorganism's identity, which have proved to be helpful for the diagnosis of infection via odour fingerprinting. The aim of this study was to determine the VOCs produced and consumed to characterize the volatile metabolism of seven isolates of different clonal complexes (CCs) of Listeria monocytogenes . For this purpose, dichloromethane extracts from the thioglycolate broth medium were analysed by gas chromatography coupled to mass spectrometry (GC/MS). Also, multivariate analyses were applied to the data obtained. Results showed that all the isolates of L. monocytogenes produced de novo isobutanol, 2-methyl-1-butanol, 3-methyl-1-butanol, 3-(methylthio)−1-propanol, acetic acid, isobutyric acid, butanoic acid, and isovaleric acid. Significant differences were found among isolates for the production amount of these volatiles, which allowed their differentiation. Thus, CC4 (ST-219/CT-3650) and CC87 (ST-87/CT-4557) showed an active volatile compounds metabolism with high consumption nitrogen and sulphur compounds and production of alcohols and acids, and CC8 (ST-8/CT-8813) and CC3 (ST-3/CT-8722) presented a less active volatile metabolism. Moreover, within the VOCs determined, huge differences were found in the production of butanol among the seven isolates analysed, being probably a good biomarker to discriminate among isolates belonging to different CCs. Hence, the analysis of volatile profile generated by the growth of L. monocytogenes in vitro could be a useful tool to differentiate among CCs isolates.
-
-
-
Impact of COVID-19 on tuberculosis services: an experience from a tertiary care hospital
More LessIntroduction. India is home to the most significant number of tuberculosis (TB) cases around the globe. The COVID-19 crisis has massively affected TB healthcare services in the country.
Hypothesis/Gap Statement. Are we sufficiently equipped to fight against TB during emergencies?
Aim. Our study aims to provide a true insight into the disruption of TB care during the pandemic period at a tertiary care hospital in India.
Methods. A retrospective observational cohort analysis was conducted on 6491 patients who accessed the TB diagnostics at the tertiary care hospital during the study period, i.e. the COVID-19 pandemic period (March 2020 to March 2021) compared with 14 665 in the control period (March 2019 to Feb 2020).
Results. Out of the total tested, 3136 patients were notified as new TB cases in the study period than 4370 in the control period (P-value=0.0000001), i.e. 28.23 % decline in notifications. A drastic decline of 69 % in notifications was observed during the lock down months in the pandemic period, i.e. March to June 2020 (P-value=0.00001). A reduction of 44 % in treatment accession by 3690 TB patients in the control period compared with 2062 in the study period (P-value=0.0000001) was noted. Lost to follow-up patients increased by 65 % from 460 in the control period to 760 in the study period (P-value=0.0000001). Also, an increased death rate by 43 % from control to study period (P-value=0.0000001) was reported.
Conclusion. There is an urgent need to maintain the continuity of essential TB services to reduce the rising burden in vulnerable populations. The need of the hour is to undertake novel strategies for tuberculosis control to combat such emergencies in the coming future.
-
- Medical Mycology
-
-
-
Practical checklist for implementation of antifungal stewardship programmes
More LessIntroduction. Antifungal stewardship programmes are needed in healthcare facilities to limit the overuse or misuse of antifungals, which are responsible for an increase in antifungal resistance.
Hypothesis/Gap Statement. Core recommendations for antifungal stewardship were published by the Mycoses Study Group Education and Research Consortium, while the Centers for Disease Control and Prevention (CDC) provided a Core Elements of Hospital Antibiotic Stewardship Programs checklist. The recommendations offer global core elements for best practices in antifungal stewardship, but do not provide a framework for the implementation of antifungal stewardship programmes in healthcare facilities.
Aim. In line with the recommendations, it is of the utmost importance to establish a practical checklist that may be used to implement antifungal stewardship programmes.
Methodology. The practical checklist was established by a national consensus panel of experts involved in antifungal stewardship activities. A preliminary checklist was sent to all experts. The final document was approved by the panel after discussion and the resolution of any disagreements by consensus.
Results. The final checklist includes the following items: leadership support; actions to support optimal antifungal use; actions to monitor antifungal prescribing, use and resistance; and an education programme.
Conclusion. This antifungal stewardship checklist offers opportunities for antifungal resistance containment, given that antifungal stewardship activities promote the optimal use of antifungals.
-
-
- Prevention, Therapy and Therapeutics
-
-
-
16S rDNA analysis of osteoporotic rats treated with osteoking
More LessIntroduction. Osteoporosis (OP) is characterized by microstructural degeneration of bone tissue, low bone mass, bone fragility and even brittle fracture (osteoporotic fracture, OPF). OP and OPF are common and there are many disadvantages to the current medications for OP/OPF. Osteoking is a traditional Chinese medicine (TCM) originating from the Yi nationality (Yunnan, China) that has been used to treat bone diseases for decades.
Hypothesis/Gap Statement. This study will reveal the changes in the intestinal microbiota of OP rats after 70 days of osteoking treatment.
Method. With duplication of sham and OP rats, eight groups were established, with six rats in each group. The intestinal microbiotas were analysed by 16S rDNA sequencing.
Results. The results showed that osteoking changed the intestinal microbiota of sham rats and OP rats. The mechanism by which osteoking improves OP is related to the functions of the intestinal microbiota. After 70 days of treatment with osteoking, the contents of Pseudonocardia, Pedomicrobium, Variovorax, Niastella and Actinosynnema were decreased in OP rats. The functions of the above intestinal microbiota related to iron metabolism affected calcifediol and 25(OH)D, and measuring these bone metabolic indicators is required for further study.
Conclusion. Osteoking changes the intestinal microbiota to improve OP, and further study which reveals these intestinal microbiota and mechanism is needed.
-
-
Volumes and issues
-
Volume 73 (2024)
-
Volume 72 (2023 - 2024)
-
Volume 71 (2022)
-
Volume 70 (2021)
-
Volume 69 (2020)
-
Volume 68 (2019)
-
Volume 67 (2018)
-
Volume 66 (2017)
-
Volume 65 (2016)
-
Volume 64 (2015)
-
Volume 63 (2014)
-
Volume 62 (2013)
-
Volume 61 (2012)
-
Volume 60 (2011)
-
Volume 59 (2010)
-
Volume 58 (2009)
-
Volume 57 (2008)
-
Volume 56 (2007)
-
Volume 55 (2006)
-
Volume 54 (2005)
-
Volume 53 (2004)
-
Volume 52 (2003)
-
Volume 51 (2002)
-
Volume 50 (2001)
-
Volume 49 (2000)
-
Volume 48 (1999)
-
Volume 47 (1998)
-
Volume 46 (1997)
-
Volume 45 (1996)
-
Volume 44 (1996)
-
Volume 43 (1995)
-
Volume 42 (1995)
-
Volume 41 (1994)
-
Volume 40 (1994)
-
Volume 39 (1993)
-
Volume 38 (1993)
-
Volume 37 (1992)
-
Volume 36 (1992)
-
Volume 35 (1991)
-
Volume 34 (1991)
-
Volume 33 (1990)
-
Volume 32 (1990)
-
Volume 31 (1990)
-
Volume 30 (1989)
-
Volume 29 (1989)
-
Volume 28 (1989)
-
Volume 27 (1988)
-
Volume 26 (1988)
-
Volume 25 (1988)
-
Volume 24 (1987)
-
Volume 23 (1987)
-
Volume 22 (1986)
-
Volume 21 (1986)
-
Volume 20 (1985)
-
Volume 19 (1985)
-
Volume 18 (1984)
-
Volume 17 (1984)
-
Volume 16 (1983)
-
Volume 15 (1982)
-
Volume 14 (1981)
-
Volume 13 (1980)
-
Volume 12 (1979)
-
Volume 11 (1978)
-
Volume 10 (1977)
-
Volume 9 (1976)
-
Volume 8 (1975)
-
Volume 7 (1974)
-
Volume 6 (1973)
-
Volume 5 (1972)
-
Volume 4 (1971)
-
Volume 3 (1970)
-
Volume 2 (1969)
-
Volume 1 (1968)
Most Read This Month