-
Volume 71,
Issue 10,
2022
-
Volume 71,
Issue 10,
2022
Volume 71, Issue 10, 2022
- Editorials
-
- Personal Views
-
-
-
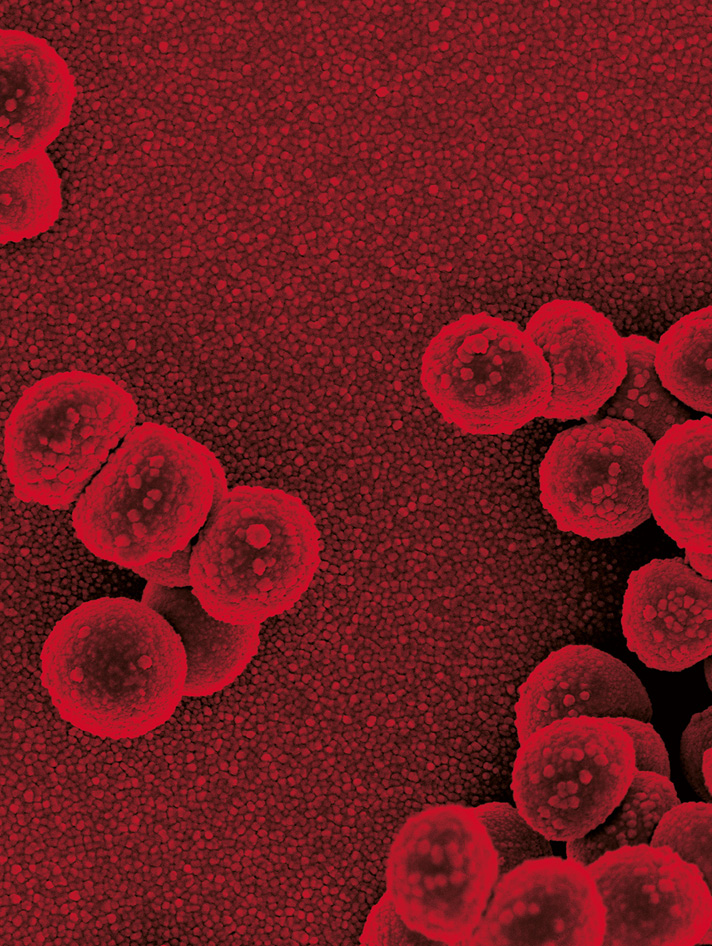
Dilemma and a way out for bacterial biofilm research
More LessBiofilm-associated infections (BAIs) are more common in clinical practice and have become a public health problem of global concern. We present our views on current research (detection methods, mechanism research, animal model construction, treatment strategies, etc.) on biofilms and BAIs, and discuss future developments concerning this important issue.
-
-
- Reviews
-
-
-
Technologies to decontaminate bacterial biofilm on hospital surfaces: a potential new role for cold plasma?
More LessHealthcare-associated infections (HCAIs) are a major challenge and the near patient surface is important in harbouring causes such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridioides difficile . Current approaches to decontamination are sub-optimal and many studies have demonstrated that microbial causes of HCAIs may persist with onward transmission. This may be due to the capacity of these microbes to survive in biofilms on surfaces. New technologies to enhance hospital decontamination may have a role in addressing this challenge. We have reviewed current technologies such as UV light and hydrogen peroxide and also assessed the potential use of cold atmospheric pressure plasma (CAPP) in surface decontamination. The antimicrobial mechanisms of CAPP are not fully understood but the production of reactive oxygen and other species is believed to be important. CAPP systems have been shown to partially or completely remove a variety of biofilms including those caused by Candida albicans, and multi-drug-resistant bacteria such as MRSA. There are some studies that suggest promise for CAPP in the challenge of surface decontamination in the healthcare setting. However, further work is required to define better the mechanism of action. We need to know what surfaces are most amenable to treatment, how microbial components and the maturity of biofilms may affect successful treatment, and how would CAPP be used in the clinical setting.
-
-
- JMM Profiles
-
-
-
JMM Profile: Staphylococcus epidermidis
More LessStaphylococcus epidermidis is the most abundant commensal bacterium of human skin. Despite protecting us from foreign invaders, S. epidermidis itself exploits human vulnerability when given the opportunity. Such opportunities arise when patients are immunocompromised or when biomedical implants present an opportunity to colonize the surface and form biofilms. S. epidermidis is one of the most frequently isolated organisms from implanted devices and from bloodstream infections. However, S. epidermidis infections are often recalcitrant to antibiotics because of biofilm-associated antibiotic tolerance. Furthermore, the emergence and spread of nearly pan-resistant strains is a considerable health concern. Symptoms can be subclinical, making diagnosis challenging, and treatment with antibiotics is inefficient. For now, infection prevention remains the best strategy available.
-
-
- Antimicrobial Resistance
-
-
-
Pharmacodynamics of colistin resistance in carbapenemase-producing Klebsiella pneumoniae: the double-edged sword of heteroresistance and adaptive resistance
More LessIntroduction. The presence of heteroresistant subpopulations and the development of resistance during drug exposure (adaptive resistance) limits colistin’s efficacy against carbapenemase-producing Klebsiella pneumoniae (CP-Kp) isolates.
Hypothesis/Gap statement. The pharmacokinetic/pharmacodynamic (PK/PD) characteristics of both types of colistin resistance against CP-Kp are unknown.
Aim. We therefore studied the PK/PD characteristics of colistin resistance in an in vitro PK/PD model simulating clinical colistin exposures.
Methods. Two K. pneumoniae clinical isolates, one non-CP-Kp and one CP-Kp, with colistin MICs of 0.5–1 mg l−1 at a final inoculum of 107 c.f.u. ml−1 were used in an in vitro PK/PD dialysis/diffusion closed model simulating 4.5 MU q12h and 3 MU q8h clinical dosing regimens. Heteroresistant (HRS, bacteria with stable high-level resistance present before drug exposure) and adaptive resistant (ARS, bacteria with reversible low-level resistance emerging after drug exposure) subpopulations were measured and optimal PK/PD targets for reducing both ARS and HRS were determined. Cumulative fractional response (CFR) was calculated with Monte Carlo simulation for 9 MU q24h, 4.5 MU q12h and 3 MU q8h clinical dosing regimens.
Results. A 2–5 log10c.f.u. ml–1 decrease of the total bacterial population was observed within the first 2 h of exposure, followed by regrowth at 12 h. Colistin exposure was positively and negatively correlated with HRS and ARS 24–0 h c.f.u. ml–1 changes, respectively. An optimal PK/PD (~0.5log10 increase) target of 35 fAUC/MIC (the ratio of the area under the unbound concentration–time curve to the MIC) was found for reducing both HRS and ARS of high-level resistance (MIC >16 mg l−1). The 4.5 MU q12h regimen had slightly higher CFR (74 %) compared to the other dosing regimens.
Conclusions. High colistin exposures reduced high-level adaptive resistance at the expense of selection of heteroresistant subpopulations.
-
-
-
-
Comparative genomics and pangenomics of vancomycin-resistant and susceptible Enterococcus faecium from Irish hospitals
More LessIntroduction. Enterococcus faecium has emerged as an important nosocomial pathogen, which is increasingly difficult to treat due to the genetic acquisition of vancomycin resistance. Ireland has a recalcitrant vancomycin-resistant bloodstream infection rate compared to other developed countries.
Hypothesis/Gap statement. Vancomycin resistance rates persist amongst E. faecium isolates from Irish hospitals. The evolutionary genomics governing these trends have not been fully elucidated.
Methodology. A set of 28 vancomycin-resistant isolates was sequenced to construct a dataset alongside 61 other publicly available Irish genomes. This dataset was extensively analysed using in silico methodologies (comparative genomics, pangenomics, phylogenetics, genotypics and comparative functional analyses) to uncover distinct evolutionary, coevolutionary and clinically relevant population trends.
Results. These results suggest that a stable (in terms of genome size, GC% and number of genes), yet genetically diverse population (in terms of gene content) of E. faecium persists in Ireland with acquired resistance arising via plasmid acquisition (vanA) or, to a lesser extent, chromosomal recombination (vanB). Population analysis revealed five clusters with one cluster partitioned into four clades which transcend isolation dates. Pangenomic and recombination analyses revealed an open (whole genome and chromosomal specific) pangenome illustrating a rampant evolutionary pattern. Comparative resistomics and virulomics uncovered distinct chromosomal and mobilomal propensity for multidrug resistance, widespread chromosomal point-mutation-mediated resistance and chromosomally harboured arsenals of virulence factors. Interestingly, a potential difference in biofilm formation strategies was highlighted by coevolutionary analysis, suggesting differential biofilm genotypes between vanA and vanB isolates.
Conclusions. These results highlight the evolutionary history of Irish E. faecium isolates and may provide insight into underlying infection dynamics in a clinical setting. Due to the apparent ease of vancomycin resistance acquisition over time, susceptible E. faecium should be concurrently reduced in Irish hospitals to mitigate potential resistant infections.
-
-
-
Comparative in vitro activities of omadacycline, eravacycline and tigecycline against non-ESBL-producing, ESBL-producing and carbapenem-resistant isolates of K. pneumoniae
More LessIntroduction. Extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae and carbapenem-resistant Enterobacteriaceae are characterized by the World Health Organization as pathogens for which new antibiotics are urgently needed. Omadacycline and eravacycline are two novel antibacterials within the tetracycline class.
Gap Statement. There are limited data regarding the comparison of the activities of omadacycline, eravacycline and tigecycline against K. pneumoniae isolates with different antimicrobial susceptibility profiles.
Aim. Our objective was to compare the in vitro activities of omadacycline, eravacycline and tigecycline against a collection of K. pneumoniae isolates, including non-ESBL-producing, ESBL-producing and carbapenem-resistant strains.
Methodology. Ninety-four K. pneumoniae isolates, including 30 non-ESBL-producing, 30 ESBL-producing and 34 carbapenem-resistant (22 carrying bla OXA-48, 12 carrying bla NDM) strains were included in the study. ESBL and carbapenemase genes were detected by conventional PCR. Omadacycline, eravacycline and tigecycline MICs were determined by the gradient diffusion method and interpreted using US Food and Drug Administration (FDA)-defined breakpoints.
Results. Overall, the percentage of tigecycline-susceptible strains (97.9 %) was higher than the percentage of omadacyline-susceptible (75.5 %) and eravacycline-susceptible (72.3 %) strains. The omadacycline and eravacycline susceptibility rates were 83.3 % among non-ESBL-producing isolates and 66.7 % among ESBL-producing isolates. The most common ESBL gene detected was blaCTX -M (90 %), followed by bla TEM (50 %) and bla SHV (50 %). The omadacycline and eravacycline susceptibility rate among isolates carrying bla TEM was 33.3 %, whereas it was 100 % among isolates that do not carry bla TEM. The omadacycline and eravacycline susceptibility rates among carbapenem-resistant isolates were 76.5 and 67.6 %, respectively. The omadacycline susceptibility rates among bla OXA-48-positive and bla NDM-positive isolates were 77.3 and 75.0 %, respectively. The eravacycline susceptibility rates among bla OXA-48-positive and bla NDM-positive isolates were 68.2 and 66.7 %, respectively. One carbapenem-resistant isolate was intermediate and one ESBL-producing isolate was resistant to tigecycline.
Conclusion. Overall, tigecycline was the most active tetracycline against isolates. Omadacycline and eravacycline showed excellent activity against ESBL-producing K. pneumoniae isolates that do not carry bla TEM. Omadacycline showed reasonable activity against carbapenem-resistant K. pneumoniae isolates carrying bla OXA-48 or bla NDM.
-
-
-
Rapid fluoroquinolone resistance detection in Pseudomonas aeruginosa using mismatch amplification mutation assay-based real-time PCR
More LessBackground. Antimicrobial resistance (AMR) is an ever-increasing global health concern. One crucial facet in tackling the AMR epidemic is earlier and more accurate AMR diagnosis, particularly in the dangerous and highly multi-drug-resistant ESKAPE pathogen, Pseudomonas aeruginosa .
Objectives. We aimed to develop two SYBR Green-based mismatch amplification mutation assays (SYBR-MAMAs) targeting GyrA T83I (gyrA248) and GyrA D87N, D87Y and D87H (gyrA259). Together, these variants cause the majority of fluoroquinolone (FQ) AMR in P. aeruginosa .
Methods. Following assay validation, the gyrA248 and gyrA259 SYBR-MAMAs were tested on 84 Australian clinical P. aeruginosa isolates, 46 of which demonstrated intermediate/full ciprofloxacin resistance according to antimicrobial susceptibility testing.
Results. Our two SYBR-MAMAs correctly predicted an AMR phenotype in the majority (83%) of isolates with intermediate/full FQ resistance. All FQ-sensitive strains were predicted to have a sensitive phenotype. Whole-genome sequencing confirmed 100 % concordance with SYBR-MAMA genotypes.
Conclusions. Our GyrA SYBR-MAMAs provide a rapid and cost-effective method for same-day identification of FQ AMR in P. aeruginosa . An additional SYBR-MAMA targeting the GyrB S466Y/S466F variants would increase FQ AMR prediction to 91 %. Clinical implementation of our assays will permit more timely treatment alterations in cases where decreased FQ susceptibility is identified, leading to improved patient outcomes and antimicrobial stewardship.
-
-
-
Trends in Stenotrophomonas maltophilia antibiotic resistance rates in the United States Veterans Affairs Health System
More LessIntroduction. Stenotrophomonas maltophilia is an important multidrug-resistant Gram-negative pathogen. While largely a hospital-acquired pathogen, there have been increasing reports of the pathogen in the community.
Gap Statement. Trends in S. maltophilia prevalence and resistance rates that include outpatient isolates are unknown.
Aim. We described recent trends in prevalence and resistance of S. maltophilia in the national Veterans Affairs (VA) Healthcare system.
Methodology. The study identified positive S. maltophilia clinical cultures among VA adult patients from 2010 to 2018 across all VA hospitals, long-term care facilities/units, and outpatient settings. Annual S. maltophilia resistance rates were evaluated. Multidrug resistant (MDR) was defined as resistance to sulfamethoxazole/trimethoprim (SMX/TMP) and minocycline or levofloxacin. Time trends were assessed with regression analyses to estimate annual average percent changes (AAPC) with 95 % confidence intervals using Joinpoint software.
Results. Over the 9 year study period, 18 285 S . maltophilia cultures were identified (57 % hospital, 3 % long-term care, 40 % outpatient). The most common source of S. maltophilia cultures were respiratory cultures (34.6 %) followed by urine cultures (30.4 %). In VA hospitals and long-term care facilities, the number of S. maltophilia cultures decreased significantly (by 5.4% and 8.4 % per year respectively). Overall, 3.1 % of isolates were MDR which remained stable over the study period. Resistance to other antibiotics assessed mostly remained stable, except SMX/TMP resistance decreased significantly by 8.5 % (2010, 15 %; 2018, 6 %) per year in VA hospitals.
Conclusion. While previous work has recognized S. maltophilia as primarily a nosocomial pathogen, the present study found that 40 % of cultures collected were among outpatients. Between 2010 and 2018, the number of positive S. maltophilia cultures decreased significantly in the national VA Healthcare System. Resistance to SMX/TMP decreased over the study period in VA hospitals and now more closely reflects previously reported resistance rates worldwide (0–10 %). MDR S. maltophilia remained stable and low in the national VA Healthcare System.
-
- Clinical Microbiology
-
-
-
Viral aetiology of acute central nervous system infections in children, Iran
More LessIntroduction. Viral infections are increasingly an important cause of central nervous system (CNS) complications.
Hypothesis/Gap Statement. There is no comprehensive insight about CNS infections due to viral agents among Iranian children.
Aim. This study aimed to investigate the viral aetiology, clinical and epidemiological profile of children with acute infections of the CNS.
Methodology. A prospective study was conducted on children at the referral hospital in Isfahan, Iran, from June 2019 to June 2020. A multiplex PCR assay was used to detect the viral causative agent in cerebrospinal fluid and throat/rectal swab samples.
Results. Among 103 patients with eligible criteria, a confirmed or probable viral aetiology was detected in 41 (39.8 %) patients, including enteroviruses – 56.1 %, herpes simplex virus 1/2 (HSV-1/2) – 31.7 %, Epstein-Barr virus – 17.1 %, varicella-zoster virus (VZV) – 9.7 %, influenza A virus (H1N1) –4.9 % and mumps – 2.4 %. There was a higher proportion of PCR-positive samples in infants than in other age groups. Encephalitis and meningoencephalitis were diagnosed in 68.3 % (28/41) and 22 % (9/41) PCR-positive cases, respectively.
Conclusion. The findings of this research provide insights into the clinical and viral aetiological patterns of acute CNS infections in Iran, and the importance of molecular methods to identify CNS viruses. HSV and VZV were identified as important causes of encephalitis in young children.
-
-
-
-
Fingerprinting of Mycobacterium tuberculosis isolates by MIRU-VNTR genotyping and detection of isoniazid resistance by real-time PCR
More LessIntroduction. Tuberculosis (TB) is a great public health problem in developing countries such as Egypt. Genotyping of Mycobacterium tuberculosis isolates has a prominent role in the field of TB prevention.
Aim. This study aimed to evaluate real-time PCR using Minor Groove Binder (MGB) probes and to identify circulating lineages/sub-lineages of M. tuberculosis and their transmission patterns.
Hypothesis. We hypothesize that MIRU-VNTR technique is efficient in identifying circulating M. tuberculosis lineages in Egypt.
Methodology. Fifty sputum specimens positive for acid-fast bacilli were included. Isoniazid (INH) resistance was detected using the 1 % proportion method. Real-time PCR using MGB-probes was used for simultaneous detection of TB infection and INH resistance. Partial sequencing of the katG gene was used to confirm INH resistance results. A standard 15 Mycobacterial Interspersed Repetitive Unit Variable Number Tandem Repeat (15-MIRU-VNTR) approach was used for genotyping through the MIRU-VNTRplus online platform.
Results. Only seven specimens showed phenotypic resistance to INH. M. tuberculosis was detected in all samples, while a mutation in the katG gene codon 315 was detected only in five samples, which were also phenotypically INH-resistant. Sequencing of the katG gene showed codon 315 mutation genotypically and phenotypically in the five INH-resistant isolates. Molecular genotyping of M. tuberculosis isolates revealed that the majority of isolates (26/50, 52 %) belonged to the S family of lineage_4. A low clustering rate (2 %) was observed among our isolates. According to the Hunter-Gaston Discriminatory Index (HGDI), 11 MIRU-VNTR loci were highly or moderately discriminative, while four loci were less polymorphic.
Conclusion. MIRU-VNTR genotyping revealed a low clustering rate with a low recent transmission rate of M. tuberculosis strains in Alexandria, Egypt.
-
-
-
Haemophilus influenzae type f in the post-Haemophilus influenzae type b vaccination era: a systematic review
More LessSince the introduction of Haemophilus influenzae (Hi) serotype b (Hib) vaccination, reports of increasing incidence rates of non-Hib serotypes have emerged. A systematic review was performed to investigate whether the Hi serotype f (Hif) incidence rate has increased globally and to describe its associated disease burden. In the post-Hib vaccine era, evidence shows that the incidence rate of Hif infection is increasing worldwide. In total 94 studies including 2 701 patients reported Hif infections. The estimated pooled incidence rate of Hif infection was 0.15/100 000 population per year (range: 0.05–0.40/100 000), with a median case fatality ratio of 14.3 %. Invasive infections most frequently presented as pneumonia (45 %), septicaemia (34 %) and meningitis (20 %). Of 191 Hif isolates, 87 % were ampicillin-susceptible. Multi-locus sequence typing revealed that Hif were relatively clonal, with the majority belonging to clonal complex 124. Hif causes invasive infections of significant variance in both severity and presentation. Globally, the Hif population shows little genetic variability and currently appears to possess low resistance to antimicrobials.
-
- Disease, Diagnosis and Diagnostics
-
-
-
Diagnosis and clinical significance of Human bocavirus 1 in children hospitalized for lower acute respiratory infection: molecular detection in respiratory secretions and serum
More LessIntroduction. Human bocavirus 1 (HBoV1) infection occurs with viral genome presence in respiratory secretions (RS) and serum, and therefore both samples can be used for diagnosis.
Gap statement. The diagnostic sensitivity of HBoV1 DNA detection in serum and the duration of DNAaemia in severe clinical cases have not been elucidated.
Aim. To determine HBoV1 DNA in serum and RS of paediatric patients hospitalized for lower acute respiratory infection (LARI) and to analyse the clinical–epidemiological features of positive cases.
Methodology. This was a prospective, transverse study. Physicians selected the clinical situations and obtained paired clinical samples (RS and serum) that were tested by PCR/qPCR for HBoV1. Positive cases were analysed considering time of specimen collection, co-detection, clinical manifestations and viral load; statistical significant level was set at α=0.05.
Results. HBoV1 was detected in 98 of 402 cases included (24 %); 18/98 (18 %) patients had the virus detectable in serum and 91/98 (93 %) in RS (P<0.001). Positivity rates were not significantly different in patients with RS and serum collected within or beyond 24 h of admission. Single HBoV1 infection was identified in 39/98 patients (40 %), three patients had HBoV1 in both clinical samples (3/39, 8 %) and 32 (32/39, 82 %) only in RS, 22 of them (69 %) with both clinical samples within 24 h of admission. Cough (P=0.001) and rhinitis (P=0.003) were significantly frequent among them and most patients were diagnosed with bronchiolitis (22/39, 56 %) and pneumonia (9/39, 23 %), which was more frequent compared to cases with co-infection (P=0.04). No significant differences were identified among patients with high, medium or low viral load of HBoV1 regarding rate of positivity in both clinical samples, the time of collection of RS and serum, co-detection, first episode of LARI, clinical manifestations, comorbidity or requirement for assisted ventilation. Intensive care unit (ICU) patients had a significantly higher frequency of detection (P<0.001) and co-detection (P=0.001) compared to patients on standard care.
Conclusions. HBoV1 is prevalent among infant patients hospitalized for LARI and including it in the standard testing can add to the aetiological diagnosis in these cases, especially for patients admitted to the ICU. HBoV1 detection in serum did not contribute significantly to the diagnosis as compared to detection in respiratory secretions.
-
-
-
-
A retrospective cross-sectional observational study of SARS-CoV-2 reinfection in La Ribera Health Department, Valencia, Spain
More LessIntroduction. The possibility of reinfection by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a widely proven fact and may have clinical implications.
Hypothesis /Gap Statement. It is not known whether there have been cases of reinfection by SARS-CoV-2 in La Ribera Health Department.
Aim. To determine whether there have been cases of reinfection by SARS-CoV-2 in La Ribera Health Department and to identify their characteristics.
Methodology. Retrospective cross-sectional observational study of cases of reinfection by SARS-CoV-2 in the population of La Ribera Department between March 2020 and February 2021. The positive baseline cohort includes all cases positive by RT-PCR for SARS-CoV-2, with reinfection cases being those that, after resolution of the first episode according to the World Health Organization (WHO) criteria, presented a new positive RT-PCR result.
Results. Out of a total of 15 687 cases with positive RT-PCR, 40 were considered to be reinfections, which meant a cumulative incidence of 0.255 % and an incidence density of 5.05 cases per 100 000 person-days. Most of the cases occurred during the highest incidence peaks of the pandemic in the department. Seventy-five per cent of the patients in these cases were older than 40 years, 42.5 % were healthcare professionals or nursing home residents and 12.5 % had an immunosuppressive comorbidity. There were no severe, critical or death cases. In the reinfection episodes, with respect to the first episode, there was a tendency to be milder, they required fewer days of hospitalization, their RT-PCR became negative earlier, they developed a greater humoral response and the sick leave period was shorter. The median period between the RT-PCR in the first episode and the RT-PCR in the second episode was 127.5 days (range: 48–301; IQR: 89.5–256.25)
Conclusions. SARS-CoV-2 reinfection cases are rare, tend to be mild and can occur within a median period of 127.5 days.
-
- Molecular and Microbial Epidemiology
-
-
-
mgpB genotyping and genetic diversity for antimicrobial resistance of Mycoplasma genitalium
More LessIntroduction. Antimicrobial resistance (AMR) among Mycoplasma genitalium is a global issue. Understanding the transmission dynamics of infection is an important factor in reducing the occurrence of AMR.
Hypothesis/Gap Statement. There is limited information on the genotyping and AMR traits of M. genitalium .
Aims. Single-locus sequence-based (SLSB) mgpB sequence typing and genetic diversity analyses of AMR M. genitalium isolated from patients in the Republic of Korea were performed to clarify the transmission dynamics and eludicate proper management.
Methodology. Sanger sequencing of mgpB, 23S rRNA, parC and gyrA genes from a total of 103 M . genitalium -positive specimens from 89 patients was carried out.
Results. Twenty-seven different mgpB genotypes (GTs) were identified; 12 had been reported previously and 15 had not. GT7 and GT8 occurred frequently (n=38, 36.89 %, and n=16, 15.53 %, respectively). The genetic diversity of the AMR-determining sites was randomly dispersed among the different GTs. However, these GTs were classified into two phylogenetically distinct clusters that were significantly correlated with patient age and genetic diversity at positions 2058 and 2059 in the 23S rRNA gene. The GTs of 20 consecutive samples from 6 patients were compared to investigate temporal changes in GTs. One specimen changed its GT during follow-up, suggesting a new infection.
Conclusions. mgpB sequence typing can be a reliable tool for epidemiological studies. Two clusters have different characteristics in terms of genetic diversity. The cluster with genetic diversity in the AMR-determining site may be explained by the high prevalence of the specimens and subsequent antimicrobial exposure during the study period.
-
-
- Pathogenesis, Virulence and Host Response
-
-
-
20S-ginsenoside Rg3 inhibits the biofilm formation and haemolytic activity of Staphylococcus aureus by inhibiting the SaeR/SaeS two-component system
More LessIntroduction. Staphylococcus aureus is a major cause of chronic diseases and biofilm formation is a contributing factor. 20S-ginsenoside Rg3 (Rg3) is a natural product extracted from the traditional Chinese medicine red ginseng.
Gap statement. The effects of Rg3 on biofilm formation and haemolytic activity as well as its antibacterial mechanism against S. aureus have not been reported.
Aim. This study aimed to investigate the effects of Rg3 on biofilm formation and haemolytic activity as well as its antibacterial action against clinical S. aureus isolates.
Methodology. The effect of Rg3 on biofilm formation of clinical S. aureus isolates was studied by crystal violet staining. Haemolytic activity analysis was carried out. Furthermore, the influence of Rg3 on the proteome profile of S. aureus was studied by quantitative proteomics to clarify the mechanism underlying its antibacterial action and further verified by reverse transcription quantitative real-time polymerase chain reaction (RT-qPCR).
Results. Rg3 significantly inhibited biofilm formation and haemolytic activity in clinical S. aureus isolates. A total of 63 with >1.5-fold changes in expression were identified, including 34 upregulated proteins and 29 downregulated proteins. Based on bioinformatics analysis, the expression of several virulence factors and biofilm-related proteins, containing CopZ, CspA, SasG, SaeR/SaeS two-component system and SaeR/SaeS-regulated proteins, including leukocidin-like protein 2, immunoglobulin-binding protein G (Sbi) and fibrinogen-binding protein, in the S. aureu s of the Rg3-treated group was downregulated. RT-qPCR confirmed that Rg3 inhibited the regulation of SaeR/SaeS and decreased the transcriptional levels of the biofilm-related genes CopZ, CspA and SasG.
Conclusions. Rg3 reduces the formation of biofilm by reducing cell adhesion and aggregation. Further, Rg3 can inhibit the SaeR/SaeS two-component system, which acts as a crucial signal transduction system for the anti-virulence activity of Rg3 against clinical S. aureus isolates.
-
-
-
-
Bacterial secretions in growth medium stimulate the mouse respiratory innate immune response
More LessIntroduction. Finding a safe innate immune response stimulator is one of the greatest challenges facing immunologists and vaccine manufacturers.
Gap statement. The role of sterile bacterial secretions (SBSs) of Pseudomonas aeruginosa in stimulating the innate immune response was not investigated previously.
Aim. The comparative effect of SBSs and bacterial cells of P. aeruginosa isolates isolated from freshwater (PAE) and infected wounds (PAC) on the respiratory tract innate immune response.
Methodology. Four test mice groups were instilled intranasally (i.n.) with 106 c.f.u of PAC, 106 c.f.u of PAE, SBS of PAC, and SBS of PAE. Two control groups were given i.n. either LB broth or PBS. Time-course changes in IL-1 beta mRNA, TNF-alpha mRNA, IL-1β and TNF-α, leukocyte count, bacterial uptake, and intracellular bacterial killing by mouse alveolar macrophages (AMs) and histological changes were examined. Lung bacterial burdens were counted in first and second test groups.
Results. The maximum level of IL-1β was seen as early as 2 h (1360±180 pg ml−1) post-instillation (i.n.) with SBS of PAC and 1 h (1910±244 pgml−1) post-instillation with SBS of PAE. The maximum level of TNF-α was seen as early as 4 h (953±192 pg ml−1) post-instillation with SBS of PAC and (1197±298 pg ml−1) post-instillation with SBS of PAE. These values were almost in line with IL-1β and TNF-α gene expression. Moderate infiltration of leukocytes in bronchoalveolar lavage (BAL) and lung sections and moderate activity of AMs (bacterial uptake and bacterial killing) were observed. The above innate immune response parameters in mice instilled i.n. with PAC and PAE were higher (P<0.05) than in the mice groups instilled i.n. with SBSs. The PAC was persistent in the lungs of mice for up to 72 h (3.5±0.22 log10 of c.f.u. g−1) and up to 48 h (2.05±0.21 log10 of c.f.u. g−1) for PAE.
Conclusion. The administration of mice with SBS i.n. stimulates cellular and molecular arms of the innate immune response in the respiratory tract, opening the door to the possibility of using SBS of P. aeruginosa as an adjuvant.
-
-
-
CRISPR-cas heterogeneity and plasmid incompatibility types in relation to virulence determinants of Shigella
More LessIntroduction. Virulence factors (VFs) are the most potent weapon in the molecular armoury of Shigella . In bacteria, the mobile genetic elements (MGEs) are contributors to the evolution of different types of clustered regularly interspaced short palindromic repeats-CRISPR associated genes (CRISPR-cas) variants and plasmid incompatibility types. The present study explored the virulence potential of Shigella in relation to the CRISPR-cas pattern and incompatibility types among the isolates.
Hypothesis/Gap Statement. The profile of the CRISPR-cas systems among clinical isolates of Shigella in India has not been reported earlier. Limited knowledge is available on the pattern of plasmid incompatibility groups among clinical isolates Shigella . The bias is always towards studying the genetic elements associated with AMR, but the present study highlights CRISPR-cas and incompatibility types among Shigella in association with virulence.
Aim. We aimed to investigate the distribution of virulence factors, CRISPR-cas pattern followed by plasmid incompatibility types among Shigella isolates.
Methodology. Between 2012–2017, a total of 187 isolates of Shigella were included in the study. The virulence genes' distribution was carried out. CRISPR-cas profiling followed by analysis of the repeats and spacers was carried out. PCR-based replicon typing was used to determine the incompatibility types. The interplay was statistically determined using STATA.
Results. The distribution of virulence genes showed varied pattern with ipaH present in all the isolates followed by ompA (93.6 %), virF (66.8 %), ial and sen (60.4 %), set1A (39.6 %) and set1B (39 %). CRISPR 1, CRISPR 3 and Cas6-Cas5 region were dominantly conserved. Twenty-two types of spacers were identified. The CRISPR3 repeat appeared to have a highly conserved sequence. CRISPR2 being the least common CRISPR type showed a strong association with an array of virulence genes (ial-set1A-set1B-virF) while CRISPR1 being the most dominant showed the least association with virulence genes (sen-virF). The dominant plasmids were found to be belonging to the inc FII group. The incompatibility groups FII, IncIγ, U, FIIS, FIIK, K, A/C, I1alpha was found to be associated with a greater number of virulence genes.
Conclusion. The isolates showed increasing diversity in their gene content that contributes to increasing heterogeneity among the isolates, which is a known virulence strategy among pathogens.
-
Volumes and issues
-
Volume 73 (2024)
-
Volume 72 (2023 - 2024)
-
Volume 71 (2022)
-
Volume 70 (2021)
-
Volume 69 (2020)
-
Volume 68 (2019)
-
Volume 67 (2018)
-
Volume 66 (2017)
-
Volume 65 (2016)
-
Volume 64 (2015)
-
Volume 63 (2014)
-
Volume 62 (2013)
-
Volume 61 (2012)
-
Volume 60 (2011)
-
Volume 59 (2010)
-
Volume 58 (2009)
-
Volume 57 (2008)
-
Volume 56 (2007)
-
Volume 55 (2006)
-
Volume 54 (2005)
-
Volume 53 (2004)
-
Volume 52 (2003)
-
Volume 51 (2002)
-
Volume 50 (2001)
-
Volume 49 (2000)
-
Volume 48 (1999)
-
Volume 47 (1998)
-
Volume 46 (1997)
-
Volume 45 (1996)
-
Volume 44 (1996)
-
Volume 43 (1995)
-
Volume 42 (1995)
-
Volume 41 (1994)
-
Volume 40 (1994)
-
Volume 39 (1993)
-
Volume 38 (1993)
-
Volume 37 (1992)
-
Volume 36 (1992)
-
Volume 35 (1991)
-
Volume 34 (1991)
-
Volume 33 (1990)
-
Volume 32 (1990)
-
Volume 31 (1990)
-
Volume 30 (1989)
-
Volume 29 (1989)
-
Volume 28 (1989)
-
Volume 27 (1988)
-
Volume 26 (1988)
-
Volume 25 (1988)
-
Volume 24 (1987)
-
Volume 23 (1987)
-
Volume 22 (1986)
-
Volume 21 (1986)
-
Volume 20 (1985)
-
Volume 19 (1985)
-
Volume 18 (1984)
-
Volume 17 (1984)
-
Volume 16 (1983)
-
Volume 15 (1982)
-
Volume 14 (1981)
-
Volume 13 (1980)
-
Volume 12 (1979)
-
Volume 11 (1978)
-
Volume 10 (1977)
-
Volume 9 (1976)
-
Volume 8 (1975)
-
Volume 7 (1974)
-
Volume 6 (1973)
-
Volume 5 (1972)
-
Volume 4 (1971)
-
Volume 3 (1970)
-
Volume 2 (1969)
-
Volume 1 (1968)
Most Read This Month