-
Volume 70,
Issue 10,
2021
-
Volume 70,
Issue 10,
2021
Volume 70, Issue 10, 2021
- JMM Profiles
-
-
-
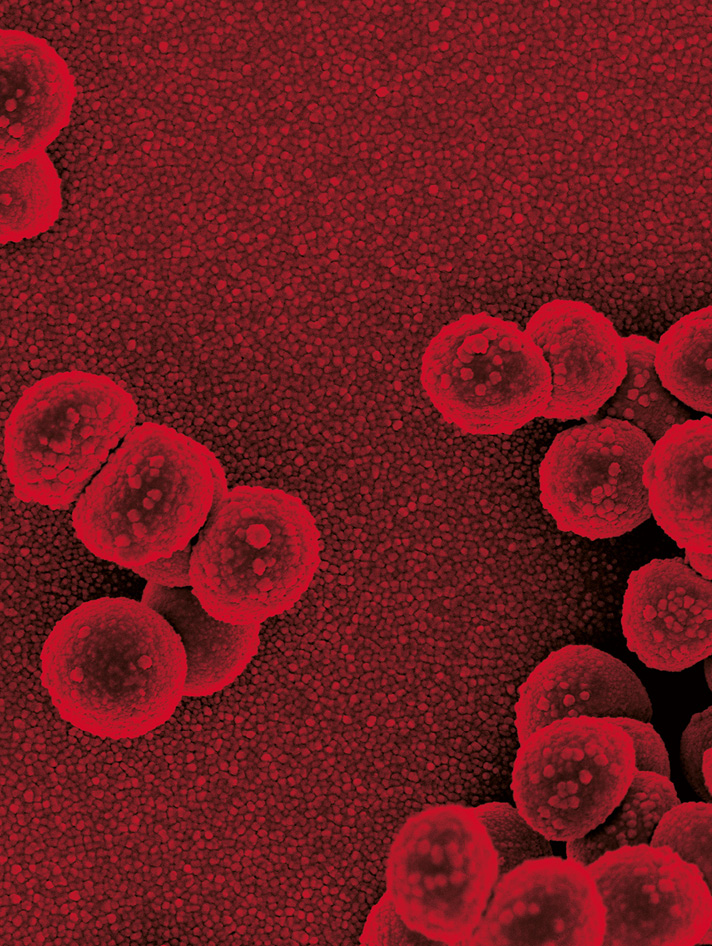
JMM Profile: Bordetella pertussis and whooping cough (pertussis): still a significant cause of infant morbidity and mortality, but vaccine-preventable
More LessWhooping cough (pertussis) is a highly contagious respiratory bacterial infection caused by Bordetella pertussis and is an important cause of morbidity and mortality worldwide, particularly in infants. Bordetella parapertussis can cause a similar, but usually less severe pertussis-like disease. Bordetella pertussis has a number of virulence factors including adhesins and toxins which allow the organism to bind to ciliated epithelial cells in the upper respiratory tract and interfere with host clearance mechanisms. Typical symptoms of pertussis include paroxysmal cough with characteristic whoop and vomiting. Severe complications and deaths occur mostly in infants. Laboratory confirmation can be performed by isolation, detection of genomic DNA or specific antibodies. Childhood vaccination is safe, effective and remains the best control method available. Many countries have replaced whole-cell pertussis vaccines (wP) with acellular pertussis vaccines (aP). Waning protection following immunisation with aP is considered to be more rapid than that from wP. Deployed by resource-rich countries to date, maternal immunisation programmes have also demonstrated high efficacy in preventing hospitalisation and death in infants by passive immunisation through transplacental transfer of maternal antibodies.
-
-
- Antimicrobial Resistance
-
-
-
Chitosan propolis nanocomposite alone or in combination with apramycin: an alternative therapy for multidrug-resistant Salmonella Typhimurium in rabbits: in vitro and in vivo study
More LessIntroduction. The emergence of multidrug-resistant Salmonella Typhimurium strains has increased the need for safe, alternative therapies from natural sources with antibacterial properties.
Hypothesis/Gap Statement. There are no published data regarding the use of chitosan propolis nanocomposite (CPNP) either alone or in combination with antibiotics as antimicrobials against S. Typhimurium, especially in Egypt.
Aim. This study evaluated the antibacterial activities of five antimicrobials [apramycin, propolis, chitosan nanoparticles (CNPs), chitosan propolis nanocomposite (CPNP) and CPNP +apramycin] against ten virulent and multidrug-resistant (MDR) S. Typhimurium field strains recovered from diarrheic rabbits through in vitro and in vivo study.
Methodology. The expression levels of three virulence genes of S. Typhimurium strains were determined by quantitative reverse-transcription PCR (RT-qPCR) after exposure to sub-inhibitory concentrations of apramycin, propolis, CNPs, CPNP alone, and CPNP +apramycin. Additionally, 90 New Zealand rabbits were divided into control and experimentally S. Typhimurium-infected groups. The infected rabbits were orally administered saline solution (infected–untreated); 10 mg apramycin/kg (infected–apramycin-treated); 50 mg propolis/kg (infected–propolis-treated); 15 mg CPNP/kg (infected–CPNP-treated) and 15 mg CPNP +10 mg apramycin/kg (infected–CPNP +apramycin-treated) for 5 days.
Results. The RT-qPCR analysis revealed different degrees of downregulation of all screened genes. Furthermore, the treatment of infected rabbits with CPNP or CPNP +apramycin significantly improved performance parameters, and total bacterial and Salmonella species counts, while also modulating both oxidative stress and altered liver and kidney parameters.
Conclusion. This work demonstrates the use of CPNP alone or in combination with apramycin in the treatment of S. Typhimurium in rabbits.
-
-
-
-
In vitro synergistic activity of aztreonam (AZT) plus novel and old β-lactamase inhibitor combinations against metallo-β-lactamase-producing AZT-resistant Enterobacterales
More LessThe emergence of metallo-β-lactamase (MBL)-producing Enterobacterales , mainly New Delhi metallo-β-lactamase (NDM), represents a clinical threat due to the limited therapeutic alternatives. Aztreonam (AZT) is stable to MBLs, but most MBL-producing Enterobacterales isolates usually co-harbour other β-lactamases that confer resistance to AZT and, consequently, its use is restricted in these isolates. We compared the ability of sulbactam (SUL), tazobactam (TAZ), clavulanic acid (CLA) and avibactam (AVI) to restore the AZT activity in MBL-producing AZT-resistant Enterobacterales isolates. A collection of 64 NDM-producing AZT-resistant Enterobacterales from five hospitals in Buenos Aires city, Argentina, were studied during the period July–December 2020. MICs were determined using the agar dilution method with Mueller–Hinton agar according to Clinical and Laboratory Standards Institute (CLSI) recommendations. AVI, SUL and TAZ were used at a fixed concentration of 4 mg l−1, whereas CLA was used at a fixed concentration of 2 mg l−1. A screening method based on disc diffusion to evaluate this synergy was also conducted. Detection of bla KPC, bla OXA, bla NDM, bla VIM, bla CTXM-1, bla PER-2 and bla CIT was performed by PCR. The AZT-AVI combination restored the AZT activity in 98.4 % of AZT-resistant strains, whereas CLA, TAZ and SUL did so in 70.3, 15.6 and 12.5 %, respectively, in isolates co-harbouring extended-spectrum β-lactamases, but were inactive in isolates harbouring AmpC-type enzymes and/or KPC. The synergy screening test showed an excellent negative predictive value to confirm the absence of synergy, but positive results should be confirmed by a quantitative method. The excellent in vitro performance of the AZT-CLA combination represents a much more economical alternative to AZT-AVI, which could be of use in the treatment of MBL-producing, AZT-resistant Enterobacterales .
-
-
-
In vitro effectiveness of biapenem against IMP-producing Enterobacteriaceae
More LessThe options available for treating infections with carbapenemase-producing Enterobacteriaceae (CPE) are limited; with the increasing threat of these infections, new treatments are urgently needed. Biapenem (BIPM) is a carbapenem, and limited data confirming its in vitro killing effect against CPE are available. In this study, we examined the minimum inhibitory concentrations (MICs) and minimum bactericidal concentrations (MBCs) of BIPM for 14 IMP-1-producing Enterobacteriaceae strains isolated from the Okayama region in Japan. The MICs against almost all the isolates were lower than 0.5 µg ml−1, indicating susceptibility to BIPM, while approximately half of the isolates were confirmed to be bacteriostatic to BIPM. However, initial killing to a 99.9 % reduction was observed in seven out of eight strains in a time–kill assay. Despite the small data set, we concluded that the in vitro efficacy of BIPM suggests that the drug could be a new therapeutic option against infection with IMP-producing CPE.
-
-
-
Quinolone-resistant uropathogenic E. coli: is there a relation between qnr genes, gyrA gene target site mutation and biofilm formation?
More LessIntroduction. The resistance to quinolone reported in uropathogenic Escherichia coli (UPEC) is commonly caused by mutations in the target site encoding genes such as the gyrA gene. Bacterial plasmids carrying resistance genes such as qnr genes can also transfer resistance. Biofilms produced by UPEC can further aid the development of resistant urinary tract infections (UTIs).
Hypothesis. Biofilm production is associated with higher prevalence of quinolones resistance genetic determinants.
Aim. To detect the prevalence of qnr genes and gyrA gene mutation among quinolone-resistant UPEC and to investigate the relation between these genetic resistance determinants and biofilm production.
Methodology. Catheterized urine samples were collected from 420 patients with evidence of UTIs and processed using standard techniques. Isolated UPEC were screened for quinolone resistance using an antimicrobial susceptibility test. Biofilm production among quinolone-resistant isolates was detected using the tissue culture plate method. All quinolone-resistant isolates were screened for qnr genes (qnrA, qnrB and qnrS) by multiplex PCR and for gyrA gene mutation by PCR-RFLP.
Results. Two hundred and sixty-four UPEC isolates were detected from 420 processed urine samples. Out of the identified 264 UPEC, 123 (46.6 %) isolates were found to be quinolone-resistant, showing resistance to 1 or more of the tested quinolones. Of the 123 quinolone-resistant UPEC detected, 71(57.7 %) were biofilm producers. The qnr genes were detected among 62.6 % of the quinolone-resistant UPEC, with an estimated prevalence of 22.8, 32.5 and 37.4 % for qnrA, qnrB and qnrS genes, respectively. Additionally, the gyrA gene mutation was identified among 53.7 % of the quinolone-resistant isolates. We reported a significant association between biofilm production and the presence of qnrA, qnrB and qnrS genes. Furthermore, the gyrA gene mutation was significantly associated with biofilm-producing isolates. The coexistence of qnr genes, gyrA gene mutation and biofilm production was demonstrated in almost 40 % of the quinolone-resistant isolates.
Conclusions. A significantly higher prevalence of qnr genes (qnrA, qnrB and qnrS) as well as the gyrA gene mutation was found among biofilm-forming UPEC. The reported coexistence of these different resistance mechanisms could aggravate quinolone resistance. Therefore, monitoring of resistance mechanisms and a proper stewardship programme are necessary.
-
-
-
In vitro activity of bedaquiline against Mycobacterium avium complex
More LessIntroduction. Nontuberculous mycobacteria (NTM) are widespread in the environment and can cause various diseases in humans, especially immunocompromised patients.
Hypothesis. Treatment of diseases caused by NTM is a complicated issue, mainly due to the resistance of the pathogen to most antimicrobial agents. Bedaquiline (Bdq) is now widely used for the treatment of multidrug-resistant (MDR) and extensively drug-resistant (XDR) tuberculosis (TB).
Aim. The main goal of our study was to evaluate the activity of Bdq against Mycobacterium avium complex (MAC), the most common species among NTM.
Methodology. A total of 166 MAC cultures (124 Mycobacterium avium and 42 Mycobacterium intracellulare ) were studied. The minimum inhibitory concentrations (MICs) of Bdq for M. avium and M. intracellulare were obtained by twofold serial dilutions in the Middlebrook 7H9 medium. MIC ranges were determined and the MIC50, MIC90 and ECOFF values were obtained.
Results. The MICs in respect of M. avium ranged from 0.003 to 1.0 µg ml−1; those for M. intracellulare ranged from 0.003 to 0.5 µg ml−1. The Bdq MIC50 and MIC90 values were found to be 0.015 and 0.12 µg ml−1 , respectively, for M. avium and 0.007 and 0.06 µg ml−1, respectively, for M. intracellulare . The tentative ECOFF values for M. avium and M. intracellulare were 0.12 and 0.06 µg ml−1, respectively.
Conclusion. The main bedaquiline susceptibility parameters for MAC strains isolated in the Moscow region were determined.
-
-
-
The epidemiology of AmpC-producing Escherichia coli isolated from dairy cattle faeces on pasture-fed farms
More LessIntroduction. Antibiotic use, particularly amoxicillin-clavulanic acid in dairy farming, has been associated with an increased incidence of AmpC-hyperproducing Escherichia coli .
Gap statement. There is limited information on the incidence of AmpC-hyperproducing E. coli from seasonal pasture-fed dairy farms.
Aim. We undertook a New Zealand wide cross-sectional study to determine the prevalence of AmpC-producing E. coli carried by dairy cattle.
Methodology. Paddock faeces were sampled from twenty-six dairy farms and were processed for the selective growth of both extended-spectrum beta-lactamase (ESBL)- and AmpC-producing E. coli . Whole genome sequence analysis was carried out on 35 AmpC-producing E. coli .
Results. No ESBL- or plasmid mediated AmpC-producing E. coli were detected, but seven farms were positive for chromosomal mediated AmpC-hyperproducing E. coli . These seven farms were associated with a higher usage of injectable amoxicillin antibiotics. Whole genome sequence analysis of the AmpC-producing E. coli demonstrated that the same strain (<3 SNPs difference) of E. coli ST5729 was shared between cows on a single farm. Similarly, the same strain (≤15 SNPs difference) of E. coli ST8977 was shared across two farms (separated by approximately 425 km).
Conclusion. These results infer that both cow-to-cow and farm-to-farm transmission of AmpC-producing E. coli has occurred.
-
-
-
Antibiotic resistance and the presence of bla CfxA and bla CSP genes in β-lactamase-producing clinical Capnocytophaga isolates from a university hospital in Japan
More LessIntroduction . Capnocytophaga species are common inhabitants of the oral cavity and can be responsible for systemic diseases in immunocompromised patients with granulocytopenia. Furthermore, it has been reported that some clinical isolates of Capnocytophaga species produce extended-spectrum β-lactamases (ESBLs).
Gap statement. Information is lacking about the types of β-lactamase genes possessed by Capnocytophaga spp. and the antimicrobial susceptibility of Capnocytophaga spp. possessing each β-lactamase gene.
Aim. The aim of this study was to investigate the presence of β-lactamase genes in clinical strains of β-lactamase-producing Capnocytophaga species isolated from clinical samples acquired at Shinshu University Hospital and examine the antimicrobial susceptibility of those strains.
Methodology. The β-lactamase-producing Capnocytophaga species (n=49) were obtained from clinical specimens. PCR assays were used to detect bla CfxA, bla CSP, bla TEM, bla CepA/CblA and transposon Tn4555 genes. Southern hybridization assays were used to detect bla CfxA and bla CSP. The minimum inhibitory concentration of some β-lactams was determined using the E-test method.
Results. PCR analysis indicated that the bla CfxA gene was present in 15 (30.6 %) and the bla CSP gene in 35 (69.3 %) of the 49 Capnocytophaga strains investigated, . Both bla CfxA and bla CSP genes were detected in a Capnocytophaga gingivalis strain. The PCR results were confirmed by Southern hybridization assays. Transposon Tn4555 was only detected in Capnocytophaga spp. harbouring the bla CfxA gene. All the β-lactamase-producing Capnocytophaga isolates were susceptible to ceftazidime–clavulanic acid, cefoxitin and imipenem. In contrast, most of the isolates were resistant to amoxicillin.
Conclusions. The clinical isolates of Capnocytophaga spp. showed a high prevalence of the bla CSP gene in Japan. The presence of the bla CSP gene was distributed in Capnocytophaga sputigena as well as other Capnocytophaga spp. These results seem to suggest the dissemination of bla CfxA and bla CSP β-lactamase genes among Capnocytophaga species.
-
- Clinical Microbiology
-
-
-
2-Alkyl-4-quinolone quorum sensing molecules are biomarkers for culture-independent Pseudomonas aeruginosa burden in adults with cystic fibrosis
More LessIntroduction. Pseudomonas aeruginosa produces quorum sensing signalling molecules including 2-alkyl-4-quinolones (AQs), which regulate virulence factor production in the cystic fibrosis (CF) airways.
Hypothesis/Gap statement. Culture can lead to condition-dependent artefacts which may limit the potential insights and applications of AQs as minimally-invasive biomarkers of bacterial load.
Aim. We aimed to use culture-independent methods to explore the correlations between AQ levels and live P. aeruginosa load in adults with CF.
Methodology. Seventy-five sputum samples at clinical stability and 48 paired sputum samples obtained at the beginning and end of IV antibiotics for a pulmonary exacerbation in adults with CF were processed using a viable cell separation technique followed by quantitative P. aeruginosa polymerase chain reaction (qPCR). Live P. aeruginosa qPCR load was compared with the concentrations of three AQs (HHQ, NHQ and HQNO) detected in sputum, plasma and urine.
Results. At clinical stability and the beginning of IV antibiotics for pulmonary exacerbation, HHQ, NHQ and HQNO measured in sputum, plasma and urine were consistently positively correlated with live P. aeruginosa qPCR load in sputum, compared to culture. Following systemic antibiotics live P. aeruginosa qPCR load decreased significantly (P<0.001) and was correlated with a reduction in plasma NHQ (plasma: r=0.463, P=0.003).
Conclusion. In adults with CF, AQ concentrations correlated more strongly with live P. aeruginosa bacterial load measured by qPCR compared to traditional culture. Prospective studies are required to assess the potential of systemic AQs as biomarkers of P. aeruginosa bacterial burden.
-
-
- Disease, Diagnosis and Diagnostics
-
-
-
Multicenter evaluation of the FilmArray Meningitis/Encephalitis assay in a routine setting
More LessIntroduction. The FilmArray Meningitis/Encephalitis (FA-ME) Panel (Biofire, Salt Lake City, Utah, US) enables fast and automated detection of 14 pathogens in cerebrospinal fluid (CSF).
Gap statement. The performance of the FA-ME panel in a real routine setting has not yet been described and could lead to better patient management in cases of good performance.
Aim. This multicenter study verified the FA-ME panel analytical performance in a routine hospital setting.
Methodology. Between April 2016 and April 2018, 454 CSF samples were analysed with the FA-ME panel and compared with routine diagnostics. In cases of discrepancy or lack of a comparator result, a profound analysis based on patient records and other laboratory results was performed.
Results. A first analysis of 65 frozen samples, suspicious for meningitis had a 89 % concordance with routine diagnostics. The limit of detection (LOD) was confirmed for all pathogens except for Streptococcus agalactiae and a strain of Haemophilus influenzae (Escherichia coli K1 and Cryptococcus gattii LOD experiments were not performed). The routine evaluation showed a positive result in 114 (25 %) clinical samples for at least one target. In three samples co-infections were found. After discrepancy analysis, overall sensitivity was 98 % (false negative FA-ME results for one HSV2, two HSV1 and two parechovirus). Four FA-ME results were considered false positive (two HHV6, one VZV and one E. coli K1), resulting in an overall specificity of >99 %. A clinical added value of the assay was seen in the diagnosis of eight cases of bacterial meningitis.
Conclusion. Because of its rapidity and ease of use, the FA-ME panel has great potential in the diagnosis of central nervous infections. Implementation can improve clinical management, but costs and analytical limitations need to be addressed to convince clinicians and laboratories of its value.
-
-
-
-
Sensitivity of the acute flaccid paralysis surveillance system for poliovirus in South Africa, 2016–2019
More LessIntroduction. Global poliovirus eradication is a public health emergency of international concern. The acute flaccid paralysis (AFP) surveillance programme in South Africa has been instrumental in eliminating polioviruses and keeping the country poliovirus free.
Gap statement. The sensitivity of surveillance for polioviruses by every African country is of global interest in the effort to ensure global health security from poliovirus re-emergence.
Aim. To describe the epidemiology of polioviruses from AFP cases and environmental samples in South Africa and to report the performance of the AFP surveillance system for the years 2016–2019 against targets established by the World Health Organization (WHO).
Methods. Stool specimens from AFP or suspected AFP cases were received and tested as per WHO guidelines. Environmental samples were gathered from sites across the Gauteng province using the grab collection method. Concentration was effected by the two-phase polyethylene glycol method approved by the WHO. Suspected polioviruses were isolated in RD and/or L20B cell cultures through identification of typical cytopathic effects. The presence of polioviruses was confirmed by intratypic differentiation PCR. All polioviruses were sequenced using the Sanger method, and their VP1 gene analysed for mutations.
Results. Data from 4597 samples (2385 cases) were analysed from the years 2016–2019. Two cases of immunodeficiency-associated vaccine-derived poliovirus (iVDPV) type 3 were detected in 2017 and 2018. A further 24 Sabin type 1 or type 3 polioviruses were detected for the 4 years. The national surveillance programme detected an average of 3.1 cases of AFP/100 000 individuals under 15 years old (2.8/100 000–3.5/100 000). The stool adequacy of the samples received was 53.0 % (47.0–55.0%), well below the WHO target of 80 % adequacy. More than 90 % of results were released from the laboratory within the turnaround time (96.6 %) and non-polio enteroviruses were detected in 11.6 % of all samples. Environmental surveillance detected non-polio enterovirus in 87.5 % of sewage samples and Sabin polioviruses in 12.5 % of samples.
Conclusion. The AFP surveillance programme in South Africa is sensitive to detect polioviruses in South Africa and provided no evidence of wild poliovirus or VDPV circulation in the country.
-
- Medical Mycology
-
-
-
Is there an optimal method to detach Candida albicans biofilm from dental materials?
More LessIntroduction. Candida albicans can produce a complex, dynamic and resistant biofilm on the surface of dental materials, especially denture base acrylic resins and temporary soft liners. This biofilm is the main aetiological factor for denture stomatitis, an oral inflammatory condition characterized by chronic and diffuse erythema and oedema of the denture bearing mucosa.
Gap Statement. There is no consensus in the literature regarding the best method to detach biofilms from dental materials. In order to assess the antifungal efficacy of new materials and treatments, the biofilm needs to be properly detached and quantified.
Aim. This study compared different methods of detaching C. albicans biofilm from denture base acrylic resin (Vipi Cril) and temporary soft liner (Softone) specimens.
Methodology. Specimens of each material were immersed in an inoculum of C. albicans SC5314 and remained for 90 min in orbital agitation at 75 r.p.m. and 37 °C. After the removal of non-adherent cells, the specimens were immersed in RPMI-1640 medium for 48 h. Biofilm formation was evaluated with confocal laser scanning microscopy (n=5). Then, other specimens (n=7) were fabricated, contaminated and immersed in 3 ml of sterile phosphate-buffered saline (PBS) and vortexed or sonicated for 1, 2, 5, or 10 min to detach the biofilm. The quantification of detached biofilm was performed by colony-forming unit (c.f.u.) ml−1 count. Results were submitted to one-way analysis of variance (ANOVA)/Tukey HSD test (α=0.05).
Results. A mature and viable biofilm was observed on the surfaces of both materials. For both materials, there was no significant difference (P>0.05) among detachment methods.
Conclusion. Any of the tested methods could be used to detach C. albicans biofilm from hard and soft acrylic materials.
-
-
-
-
Multi-locus sequence typing reveals genotypic similarity in Nigerian Cryptococcus neoformans AFLP1/VNI of environmental and clinical origin
More LessIntroduction
Pigeon droppings are among the major environmental sources of Cryptococcus neoformans AFLP1/VNI, from where the organism infects susceptible humans and animals resulting in cryptococcosis. Until now, C. neoformans AFLP1B/VNII was the only molecular type reported in Nigeria. Effective clinical treatment of this infection has occasionally been stymied by the emergence of antifungal non-susceptible, and resistant strains of C. neoformans AFLP1/VNI.
Hypothesis/Gap Statement
Pigeon droppings harbour C. neoformans and HIV/AIDS patients are among the susceptible population to develop cryptococcal infection. Epidemiological data on cryptococcal prevalence is limited in Nigeria.
Aim
To investigate the environmental prevalence of C. neoformans in South-eastern Nigeria and compare the isolates with other lineages by using molecular and microbiological tools.
Methodology
A total of 500 pigeon droppings and 300 blood samples of HIV/AIDS patients were collected, respectively, from five market squares and three tertiary healthcare centres within the Nsukka area of South-eastern Nigeria. The antifungal susceptibility of the C. neoformans isolates to amphotericin B, fluconazole, 5-fluorocytosine, itraconazole, voriconazole, posaconazole, and isavuconazole was investigated based on the CLSI M27-A3 protocol. Yeasts were identified by MALDI-TOF MS, thereafter Cryptococcus MLST was performed according to the International Society for Human and Animal Mycology (ISHAM) consensus scheme.
Results
C. neoformans was recovered from 6 (1.2 %) pigeon droppings and 6 (2 %) blood cultures of HIV/AIDS patients. Molecular analyses indicated that all cryptococcal isolates belong to serotype A and the AFLP1/VNI molecular type with sequence type (ST)32. Infection with C. neoformans was independent of sex and age of the patients investigated. All C. neoformans isolates were susceptible to the seven antifungal agents.
Conclusion
This is the first report on the prevalence of C. neoformans AFLP1/VNI (ST32) in environmental and clinical samples from Nigeria. The antifungal susceptibility indicates that antifungal resistance by C. neoformans is yet a rare occurrence in Nigeria.
-
- Microbiome and Microbial Ecology in Health
-
-
-
Evaluation of Culture Top transport systems for assessing the bacterial diversity of microbiota by culturomics as compared to a routine transport system
More LessIn recent years, metagenomics and then culturomics, which consists of the multiplication of media and culture conditions and the rapid identification of all bacterial colonies, have generated renewed interest in the human microbiota, and diseases associated with modifications in its composition in particular. The sample transport media included in diverse swab transport systems and the storage conditions are among the factors that influence the results of the culturomics. In this study, we compared the results of culturomics from paired skin, oral and rectal swabs from intensive care unit (ICU) patients using Culture Top sample transport medium as compared to our routine one. From 152 clinical samples, we were able to isolate and identify 45 600 colonies, belonging to 338 different bacterial species. The transport system Culture Top identified 282 different bacterial species, while 244 were identified by our routine system. Of these, 188 different bacterial species were commonly identified using both transport systems, while 94 (27.8 %) and 56 (16.5 %) were only identified using Culture Top and our routine system, respectively (P<0.001), but there was no significant difference in bacterial diversity at the genus or phylum level, or in terms of their type of respiration and cell wall. In conclusion, the Culture Top transport system appears to be complementary to our routine system, although it seems slightly superior in terms of isolated bacterial species.
-
-
-
-
The role of Akkermansia muciniphila in obesity, diabetes and atherosclerosis
More LessAlteration in the composition of the gut microbiota can lead to a number of chronic clinical diseases. Akkermansia muciniphila is an anaerobic bacteria constituting 3–5% of the gut microbial community in healthy adults. This bacterium is responsible for degenerating mucin in the gut; its scarcity leads to diverse clinical disorders. In this review, we focus on the role of A. muciniphila in diabetes, obesity and atherosclerosis, as well as the use of this bacterium as a next-generation probiotic. In regard to obesity and diabetes, human and animal trials have shown that A. muciniphila controls the essential regulatory system of glucose and energy metabolism. However, the underlying mechanisms by which A. muciniphila alleviates the complications of obesity, diabetes and atherosclerosis are unclear. At the same time, its abundance suggests improved metabolic disorders, such as metabolic endotoxemia, adiposity insulin resistance and glucose tolerance. The role of A. muciniphila is implicated in declining aortic lesions and atherosclerosis. Well-characterized virulence factors, antigens and cell wall extracts of A. muciniphila may act as effector molecules in these diseases. These molecules may provide novel mechanisms and strategies by which this bacterium could be used as a probiotic for the treatment of obesity, diabetes and atherosclerosis.
-
- Molecular and Microbial Epidemiology
-
-
-
Carbapenem-resistant Klebsiella pneumoniae colonization and infection is associated with lower overall survival in a cohort of haematopoietic stem-cell transplantation patients: mechanism of resistance and virulence by whole-genome sequencing
More LessCarbapenem-resistant Klebsiella pneumoniae (CRK) infections are a growing concern in immunocompromised patients. The aim of the present study was to evaluate the impact of CRK colonization and infection in overall mortality for haematopoietic stem-cell transplant (HSCT) patients. We also aimed to investigate resistance and virulence profiles of CRK isolates and assess their epidemiological and genetic relatedness. Patients in the HSCT unit were screened for colonization with CRK with weekly rectal swab or stool cultures and placed under contact precautions. We defined CRK colonization as positive culture from a swab or stool sample grown in MacConkey agar with meropenem at 1 µg ml−1. Demographic and clinical data were retrieved from the patients’ charts and electronic records. According to resistance mechanisms and pulsed field gel electrophoresis profile, isolates were selected based on whole-genome sequencing (WGS) using MiSeq Illumina. Outcomes were defined as overall mortality (death up to D+100), and infection-related death (within 14 days of infection). We report a retrospective cohort of 569 haematopoietic stem-cell transplant patients with 105 (18.4 %) CRK colonizations and 30 (5.3 %) infections. blaKPC was the most frequent carbapenemase in our cohort with three isolates co-harbouring blaKPC and blaNDM. We found no difference in virulence profiles from the CRK isolates. There were also no significant differences in virulence profiles among colonization and infection isolates regarding genes encoding for type 1 and 3 fimbriae, siderophores, lipopolysaccharide and colibactin. In clonality analysis by PFGE and WGS, isolates were polyclonal and ST340 was the most prevalent. Overall survival at D+100 was 75.4 % in in CRK-colonized (P=0.02) and 35.7 % in infected patients and significantly lower than non-colonized patients (85.8 %; P<0.001). We found a higher overall mortality associated with colonization and infection; KPC was the main resistance mechanism for carbapenems. The polyclonal distribution of isolates and findings of CRK infection in patients not previously colonized suggest the need to reinforce antibiotic stewardship.
-
-
-
-
Emergence of novel strains of Shigella flexneri associated with sexual transmission in adult men in England, 2019–2020
More LessNational surveillance of shigellosis in England revealed an increase in sexually transmitted Shigella flexneri in adult males in 2019 that persisted throughout 2020. We observed a resurgence of azithromycin-resistant S. flexneri serotype 3a, and the emergence of two novel multidrug-resistant clades of S. flexneri 2a and S. flexneri 1b.
-
-
-
High seroprevalence of anti-DENV IgM in blood donors in an early outbreak in the Federal District of Brazil, 2019
More LessDengue is endemic in Brazil, and several Brazilian cities are affected by frequent seasonal outbreaks of the disease. During the outbreaks the possibility of transfusion-transmitted dengue (TTD) is increased, mainly by the presence of asymptomatic or oligosymptomatic infections in eligible blood donors. The retrospective assessment of anti-DENV IgM and NS1 seroprevalence during a given time interval may indicate the need for measures for the previous screening of DENV infection in blood donors. In this context, we performed retrospective screening for anti-DENV IgM and NS1 in blood donors from the Federal District of Brazil during the early outbreak that occurred in 2019, the largest outbreak in recent years. In total, 450 blood donations were screened for anti-DENV IgM and DENV NS1 using commercial enzyme-linked immunosorbent assay kits (Panbio Dengue IgM Capture ELISA and Platelia Dengue NS1 Ag, respectively). Among the tested plasma samples, 16 % (72/450) presented anti-DENV IgM; no samples presented DENV NS1. Despite the apparent absence of antigenaemia in tested blood donations, the high prevalence of anti-DENV IgM highlights the importance of DENV screening in blood donors, principally during outbreak periods.
-
- Pathogenesis, Virulence and Host Response
-
-
-
The antiviral drug efavirenz reduces biofilm formation and hemolysis by Staphylococcus aureus
More LessIntroduction. Biofilm formation and hemolysis are closely related to the pathogenicity of Staphylococcus aureus .
Hypothesis/Gap Statement. Strategies that reduce the mortality of S. aureus infections may involve novel antimicrobials and/or drugs that decrease S. aureus virulence, such as biofilm formation. The antiviral drug efavirenz is a non-nucleoside reverse transcriptase inhibitor, which also has shown antibacterial effect on Bacillus subtilis and Escherichia coli . Its effect on pathogen virulence has not yet been explored.
Aim. This study investigates the antimicrobial and anti-virulence effect of efavirenz on S. aureus .
Methodology. Biofilm biomasses were detected by crystal violet staining. Hemolysis activities of S. aureus were determined by rabbit erythrocytes lysis assay. RNA levels of transcriptional regulatory genes, biofilm-related genes, and virulence-related genes of S. aureus were determined by RT-qPCR.
Results. Efavirenz showed an inhibitory effect on the growth of S. aureus , Enterococcus faecalis and Streptococcus agalactiae at 50 µM. Efavirenz significantly inhibited biofilm formation of both methicillin-sensitive S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA) at 25 µM, but did not affect the growth of planktonic S. aureus cells. Moreover, hemolysis by S. aureus was inhibited by efavirenz at 25 µM. The expression levels of RNA transcriptional regulatory genes (agrA, agrC, sigB, saeR and saeS), biofilm-related genes (cidA, clfA, clfB, fnbA, fnbB), and virulence-related genes (hla, hld, staphopain B, alpha-3 PSM, beta PSM, delta PSM) of S. aureus decreased significantly at 25 µM efavirenz.
Conclusion. Efavirenz inhibits S. aureus biofilm formation and virulence in vitro.
-
-
- Prevention, Therapy and Therapeutics
-
-
-
Clinical efficacy and safety of antifungal drugs for the treatment of Candida parapsilosis infections: a systematic review and network meta-analysis
More LessAntifungal drugs have already been established as an effective treatment option for Candida parapsilosis infections, but there is no universal consensus on the ideal target for clinical efficacy and safety of antifungal drugs for the treatment of C. parapsilosis infections. Few studies have directly compared the efficacies of antifungal drugs for the treatment of C. parapsilosis infections. We hypothesize that different antifungal drugs offer differing clinical efficacy and safety for the treatment of C. parapsilosis infections. We performed a comprehensive network meta-analysis on different strategies for C. parapsilosis infection treatment and compared the clinical efficacy and safety of antifungal drugs as interventions for C. parapsilosis infections. The Cochrane Database of Systematic Reviews, Medline, Embase, PubMed, Web of Science, China National Knowledge Infrastructure (CNKI), Technology of Chongqing VIP database, Wan Fang Data, and SinoMed databases were searched to identify appropriate randomized trials. Among the extracted C. parapsilosis cases, the survival and death rates with treatment of C. parapsilosis infection were compared among groups treated with different antifungal drugs. According to the evidence-network analysis, echinocandins were a better choice than other drugs for treating C. parapsilosis infections, and more importantly, caspofungin showed a more preferable effect for decreasing the risk of 30 day mortality. In conclusion, this study systematically evaluated the effectiveness and safety of antifungal drugs for the purpose of helping clinicians choose the most appropriate antifungal drugs. Future studies with larger samples are needed to evaluate the effects of patient factors on the clinical efficacy and safety of antifungal drugs for C. parapsilosis infections.
-
-
Volumes and issues
-
Volume 73 (2024)
-
Volume 72 (2023 - 2024)
-
Volume 71 (2022)
-
Volume 70 (2021)
-
Volume 69 (2020)
-
Volume 68 (2019)
-
Volume 67 (2018)
-
Volume 66 (2017)
-
Volume 65 (2016)
-
Volume 64 (2015)
-
Volume 63 (2014)
-
Volume 62 (2013)
-
Volume 61 (2012)
-
Volume 60 (2011)
-
Volume 59 (2010)
-
Volume 58 (2009)
-
Volume 57 (2008)
-
Volume 56 (2007)
-
Volume 55 (2006)
-
Volume 54 (2005)
-
Volume 53 (2004)
-
Volume 52 (2003)
-
Volume 51 (2002)
-
Volume 50 (2001)
-
Volume 49 (2000)
-
Volume 48 (1999)
-
Volume 47 (1998)
-
Volume 46 (1997)
-
Volume 45 (1996)
-
Volume 44 (1996)
-
Volume 43 (1995)
-
Volume 42 (1995)
-
Volume 41 (1994)
-
Volume 40 (1994)
-
Volume 39 (1993)
-
Volume 38 (1993)
-
Volume 37 (1992)
-
Volume 36 (1992)
-
Volume 35 (1991)
-
Volume 34 (1991)
-
Volume 33 (1990)
-
Volume 32 (1990)
-
Volume 31 (1990)
-
Volume 30 (1989)
-
Volume 29 (1989)
-
Volume 28 (1989)
-
Volume 27 (1988)
-
Volume 26 (1988)
-
Volume 25 (1988)
-
Volume 24 (1987)
-
Volume 23 (1987)
-
Volume 22 (1986)
-
Volume 21 (1986)
-
Volume 20 (1985)
-
Volume 19 (1985)
-
Volume 18 (1984)
-
Volume 17 (1984)
-
Volume 16 (1983)
-
Volume 15 (1982)
-
Volume 14 (1981)
-
Volume 13 (1980)
-
Volume 12 (1979)
-
Volume 11 (1978)
-
Volume 10 (1977)
-
Volume 9 (1976)
-
Volume 8 (1975)
-
Volume 7 (1974)
-
Volume 6 (1973)
-
Volume 5 (1972)
-
Volume 4 (1971)
-
Volume 3 (1970)
-
Volume 2 (1969)
-
Volume 1 (1968)
Most Read This Month