-
Volume 68,
Issue 6,
2019
-
Volume 68,
Issue 6,
2019
Volume 68, Issue 6, 2019
- Review
-
-
-
Host- and pathogen-dependent susceptibility and predisposition to dermatophytosis
More LessDermatophytes are a highly specialized group of keratinophilic and keratinolytic filamentous fungi causing a ringworm disease called dermatophytosis or superficial mycoses. Although dermatophyte infections do not threaten the host’s life, they lower its quality in humans by causing discomfort related to cosmetic problems and through their epidemiological significance, whereas in farm animals they are responsible for economic losses and constitute a source of the spread of spores. Evidence from countless observational studies that have been conducted over the last 90 years indicates that dermatophytes infect humans of every age, race, gender and socioeconomic status with strikingly high rates, as well as both farmed and wild animals in various health conditions and with various epidemiological statuses. However, the prevalence of superficial fungal infections is highly variable, since it depends on several parameters associated with the infected individual and the dermatophyte, their mutual interactions, and epidemiological and geographical factors. The curious disparity in dermatophyte infection patterns has prompted many investigators to search for a link between the host, the host’s predispositions and susceptibility to the disease, and the dermatophyte species and virulence. Thus, the question arises as to whether, in addition to the generally recognized factors predisposing hosts to diseases, there are some other predispositions to dermatophyte infections in a species-specific host. In this review, we describe recent findings about the mechanism of dermatophyte infections, focusing on the adaptation of the fungi to the host and conditions predisposing each side to the disease.
-
-
- Antimicrobial Resistance
-
-
-
Evaluation of risk factors for colistin resistance among uropathogenic isolates of Escherichia coli and Klebsiella pneumoniae: a case–control study
More LessIntroduction. The last few years have seen the emergence of multi-drug resistant (MDR) Gram-negative infections, which are associated with high morbidity and mortality. The indiscriminate use of colistin has led to the development of resistance, which can be diagnosed effectively by broth microdilution. Studies from India are limited, and this study was conducted in order to determine the prevalence and risk factors associated with colistin resistance.
Methods. Urine samples from patients admitted with urinary tract infection (UTI), growing MDR Escherichia coli and Klebsiella pneumoniae , were tested for the minimum inhibitory concentration (MIC) of colistin by broth microdilution. Isolates with an MIC >2 µg ml−1 (resistant) were subjected to polymerase chain reaction (PCR) for the mcr1, mcr2 and mgrB genes. A case–control study with 21 cases (resistant) and 42 matched controls (sensitive) was designed to evaluate risk factors and outcomes (recurrent UTI, readmission and hospital stay >2 weeks).
Results. Two hundred and fifty MDR isolates ( E. coli =142/2319 and K.pneumoniae=108/775) from 216 patients were selected from the 25 046 isolates screened. Twenty-five isolates (20 K.pneumoniae and 5 E. coli ) were resistant to colistin, with a prevalence of 3.52 % in E. coli and 18.5 % in K. pneumoniae among the MDR isolates. PCR for the mcr1 and mcr2 genes was negative. Multivariate regression showed that multiple episodes of hospitalization, hospital stay >2 weeks, exposure to >three antibiotic classes and abnormality/surgery of the lower urinary tract were the significant risk factors for colistin resistance. Previous use of colistin and colistin resistance had a significant effect on all outcomes.
Conclusions. K. pneumoniae show six times higher prevalence of colistin resistance than E. coli , and the emergence of resistant organisms has led to an increase in morbidity in infected patients.
-
-
-
-
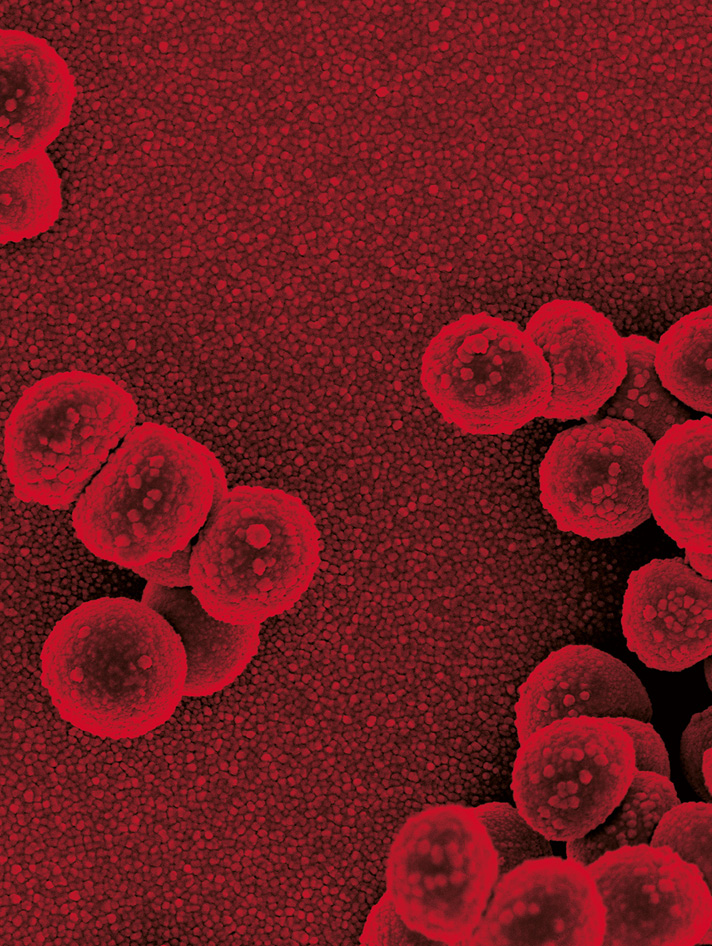
Reduced vancomycin susceptibility and increased macrophage survival in Staphylococcus aureus strains sequentially isolated from a bacteraemic patient during a short course of antibiotic therapy
More LessPurpose. The purpose of the present study was to determine the relatedness of Staphylococcus aureus strains successively isolated over a 7-day period from a single bacteraemic patient undergoing antibiotic treatment with vancomycin.
Methods. The S. aureus strains had been isolated and sequenced previously. Antibiotic susceptibility testing, population analysis profiling, and lysostaphin sensitivity and phagocytic killing assays were used to characterize these clonal isolates.
Results. The seven isolates (MEH1–MEH7) were determined to belong to a common multilocus sequence type (MLST) and spa type. Within the third and fifth day of vancomycin treatment, mutations were observed in the vraS and rpsU genes, respectively. Population analysis profiles revealed that the initial isolate (MEH1) was vancomycin-susceptible S. aureus (VSSA), while those isolated on day 7 were mostly heteroresistant vancomycin-intermediate S. aureus (hVISA). Supporting these findings, MEH7 was also observed to be slower in growth, to have an increase in cell wall width and to have reduced sensitivity to lysostaphin, all characteristics of VISA and hVISA strains. In addition, MEH7, although phagocytosed at numbers comparable to the initial isolate, MEH1, survived in higher numbers in RAW 264.7 macrophages. Macrophages infected with MEH7 also released more TNF-α and IFN-1β.
Conclusion. We report an increasing resistance to vancomycin coupled with daptomycin that occurred within approximately 3 days of receiving vancomycin and steadily increased until the infection was cleared with an alternative antibiotic therapy. This study reiterates the need for rapid, efficient and accurate detection of hVISA and VISA infections, especially in high-bacterial load, metastatic infections like bacteraemia.
-
-
-
Circulation of imipenem-resistant Acinetobacter baumannii ST10, ST2 and ST3 in a university teaching hospital from Tehran, Iran
More LessPurpose. Multi-drug resistant (MDR) Acinetobacter baumannii has introduced a worldwide health crisis. The purposes of this study were to characterize the clonal relatedness among MDR clinical strains and to introduce a new two-locus typing method confirmed by multi-locus sequence typing (MLST).
Methodology. In this study, we determined antimicrobial resistance, detected genes associated with carbapenem resistance and characterized clonal relatedness among 99 clinical isolates extracted from 82 hospitalized inpatients in a university hospital.
Results. Of the 99 A. baumannii isolates, 92.9% (92/99) were resistant to imipenem and 97.9% (97/99) had an MDR profile. We found that the high prevalence of blaVIM [94.9% (94/99)] and blaOXA-23-like [93.93% (93/99)] is the main mechanism of carbapenem resistance. This study proposes a new two-locus typing (blaOXA-51-like and ampC) method for the rapid identification of clonal complexes (CCs). The results of this method and confirmation by MLST show that clinical isolates carry blaOXA-68 as well as ampC-10 or ampC-20 genes belonging to CC10 (ST10); blaOXA-66 and ampC-2 belonging to CC2 (ST2); and blaOXA-71 and ampC-3 belonging to CC3 (ST3). One isolate had blaOXA-90 with an undetermined allele number of ampC belonging to ST513.
Conclusion. The high prevalence of MDR strains and the circulation of four limited clones, including ST10 (45/99), ST2 (41/99), ST3 (12/99) and ST513 (1/99), in the clinical setting highlights the importance of a rigorous infection control programme. The two-locus typing method has more discrimination than the application of each method separately and it could be applied for the rapid determination of the CC without performing MLST.
-
-
-
Whole genome sequencing of NDM-1-producing serotype K1 ST23 hypervirulent Klebsiella pneumoniae in China
More LessBao-Tao Liu and Wei-Qi SuPurpose. The emergence and spread of carbapenem-resistant hypervirulent Klebsiella pneumoniae (CR-hvKP) is causing worldwide concern, whereas NDM-producing hvKP is still rare. Here we report the complete genome sequence characteristics of an NDM-1-producing ST23 type clinical hvKP in PR China.
Methodology. Capsular polysaccharide serotyping was performed by PCR. The complete genome sequence of isolate 3214 was obtained using both the Illumina Hiseq platform and Pacbio RS platform. Multilocus sequence type was identified by submitting the genome sequence to mlst 2.0 and the antimicrobial resistance genes and plasmid replicons were identified using ResFinder and PlasmidFinder, respectively. Transferability of the bla NDM-1-bearing plasmid was determined by conjugation experiment, S1 pulsed-field gel electrophoresis and Southern hybridization.
Results. Isolate 3214 was classified to ST23 and belonged to the K1 capsular serotype. The isolate’s total genome size was 6 171 644 bp with a G+C content of 56.39 %, consisting of a 5 448 209 bp chromosome and seven plasmids. The resistome included 18 types of antibiotic resistance genes. Fourteen resistance genes including bla NDM-1 and bla CTX-M-14 were located on plasmids and five also including bla CTX-M-14 were in the chromosome. Plasmid pNDM_3214 carrying bla NDM-1 harboured six types of resistance genes surrounded by insertion sequences and was conjugative. The worldwide pLVPK-like virulence plasmid harbouring rmpA2 and rmpA was also found in this isolate.
Conclusion. This study provides basic information of phenotypic and genomic features of ST23 CR-hvKP isolate 3214. Our data highlights the potential risk of spread of NDM-1-producing ST23 hvKP.
-
-
-
Erythromycin-resistant Streptococcus pneumoniae: phenotypes, genotypes, transposons and pneumococcal vaccine coverage rates
More LessPurpose. To assess the antibiotic resistance, transposon profiles, serotype distribution and vaccine coverage rates in 110 erythromycin-resistant S. pneumoniae clinical isolates.
Methodology. Erythromycin, clindamycin, tetracycline, chloramphenicol and kanamycin susceptibilities were assessed using the E-test/disc diffusion method. Inducible macrolide resistance was tested using the erythromycin-clindamycin double disc diffusion test. Serogrouping and serotyping were performed using latex particle agglutination and the Quellung reaction, respectively. Drug resistance genes and transposon-specific genes were investigated by PCR.
Results. Of the isolates, 93 % were resistant to clindamycin; 81 % were resistant to tetracycline; 76 % were multi-drug-resistant, having resistance to both clindamycin and tetracycline; and 12 % had extended-drug resistance, being resistant to clindamycin, tetracycline, chloramphenicol and kanamycin. The majority of isolates (88.2 %) exhibited the cMLSB phenotype. The association between the cMLSB phenotype and tetracycline resistance was related to transposons Tn2010 (38.2 %), Tn6002 (21.8 %) and Tn3872 (18.2 %). M and iMLSB phenotypes were observed in 7 and 5 % of the isolates, respectively. The most frequent serotype was 19 F (40 %). Among the erythromycin-resistant pneumococci, vaccine coverage rates for the 13-valent pneumococcal conjugate vaccine (PCV-13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV-23) were 76.4 and 79.1 %, respectively, compared to 82.2 and 85.1 % transposon-carrying isolates.
Conclusions. Multi-drug resistance among erythromycin-resistant S. pneumoniae isolates mainly occurs due to the horizontal spread of the Tn916 family of transposons. The majority of the transposon-carrying isolates are covered by 13- and 23-valent pneumococcal vaccines. Since serotype distribution and transposons in S. pneumoniae isolates may change over time, close monitoring is essential.
-
- Clinical Microbiology
-
-
-
Dissemination of Klebsiella pneumoniae ST11 isolates with carbapenem resistance in integrated and emergency intensive care units in a Chinese tertiary hospital
More LessPurpose. The aim of the present study was to investigate the dissemination of carbapenem-resistant Klebsiella pneumoniae (CRKP) isolates in integrated intensive care units (IICUs) and emergency ICUs (EICUs) for controlling the spread of CRKP in different ICUs of the hospital.
Methodology. From January 2016 to April 2017, a total of 46 non-duplicate CRKP isolates were consecutively isolated from a tertiary hospital. The production of carbapenemases was determined by the modified carbapenem inactivation method (mCIM) test. The resistance and virulence-associated genes were detected by PCR and DNA sequencing. A hypermucoviscosity phenotype was identified by the string test. Bacterial clonal relatedness of the CRKP isolates tested was determined by multi-locus sequence typing (MLST) and PFGE.
Results. All CRKP isolates showed multiple drug resistance. All CRKP isolates harboured bla KPC-2-encoding carbapenemase and at least one of the other β-lactamase genes tested, with positive rates of 89.1 % (41/46) for bla CTX-M-65. qnrS was found among 76.1 % (35/46) of the CRKP isolates. A hypermucoviscosity phenotype was found in only two (4.3 %, 2/46) CRKP isolates. The virulence-associated genes with positive rates of more than 90 % among the 46 isolates tested included wabG (100 %, 46/46), ycf (100 %, 46/46), ureA (95.6 %, 44/46) and fim H (95.6 %, 44/46). MLST results showed that 46 CRKP isolates belonged to ST11 (95.6 %, 44/46) and ST86 (4.4 %, 2/46). PFGE patterns showed four clusters.
Conclusion. The CRKP ST11 clone with co-production of CTX-M-65 and KPC-2 disseminated in ICUs of this tertiary teaching hospital in central China. The emergence of CRKP with a hypermucoviscosity phenotype in ICUs should be of particular concern.
-
-
-
-
The importance of considering the neglected intestinal protozoan parasite Dientamoeba fragilis
More LessDientamoebiasis is globally distributed and detected in a large number of subjects with diarrhea, abdominal discomfort, flatulence, fatigue and loss of appetite. The life cycle and transmission of Dientamoeba fragilis are poorly understood. Microscopic examination of permanent stained smears is traditionally employed to diagnose the infection. However, this approach is time-consuming and the success in detecting D. fragilis depends on the microscopist’s experience. Hence, only a few laboratories routinely carry out tests for D. fragilis. Consequently, the prevalence of D. fragilis infection is probably underestimated. Although novel, rapid and more sensitive diagnostic tests are becoming available for detecting intestinal parasites, they also possess some limitations. The aim of this study was to emphasize the importance of performing microscopic examination of permanent stained smears from at least one fresh stool specimen after sample arrival at the laboratory, as a mandatory practice for the diagnosis of dientamoebiasis, particulary where it is not possible to perform molecular assays.
-
-
-
Prevalence of in vitro synergistic antibiotic interaction between fosfomycin and nonsusceptible antimicrobials in carbapenem-resistant Pseudomonas aeruginosa
More LessPurpose. We assessed the synergistic potential of fosfomycin and parenteral antibiotics among carbapenem-resistant Pseudomonas aeruginosa (CRP).
Methodology. Minimum inhibitory concentrations (MICs) were determined by broth microdilution for all antibiotics except fosfomycin, for which the gradient diffusion strip (GDS) method was used. The GDS cross method was performed to assess interactions between fosfomycin and: aztreonam, cefepime, ceftazidime, ceftazidime/avibactam, ceftolozane/tazobactam, meropenem, piperacillin/tazobactam and tobramycin. Only organisms that were nonsusceptible to the second drug were assessed.
Results. Among 153 clinical isolates, the fosfomycin MIC50/90 was 48/≥1024 mg l−1 . Synergy was detected in 131/604 (21.7 %) fosfomycin–antibiotic combinations among 76 (49.7 %) isolates. Ceftazidime (42/81, 51.9%) and ceftolozane/tazobactam (7/14, 50.0%) displayed synergy most frequently. Meropenem susceptibility was restored in 21 (13.7 %) isolates. Antagonism was not observed.
Conclusion. Fosfomycin synergy was commonly observed in vitro among CRP. These data may guide the selection of combination antibiotic therapy. The susceptibility to other antibiotics was restored in combination with fosfomycin, warranting further in vivo evaluation.
-
-
-
The incidence and patient outcomes of ABSSSI by iclaprim MIC values in the phase 3 REVIVE trials for treatment of acute bacterial skin and skin structure infections
More LessThe incidence and patient outcomes of Staphylococcus aureus isolates by iclaprim MIC was determined among patients from two phase 3 studies for the treatment of acute bacterial skin and skin structure infections (ABSSSI), REVIVE-1 and -2. Iclaprim MIC90 values were 0.12 µg ml−1 for S. aureus (0.12 µg ml−1 against methicillin-sensitive and 0.25 µg ml−1 against methicillin-resistant S. aureus ). The incidence of culture confirmed S. aureus isolates among patients with ABSSSI with an iclaprim MIC > 8 µg ml−1 was 2.0 % (16/790). The clinical outcomes varied by MICs for early clinical response (63–100 %), end of therapy response (81–100 %) and the test of cure response (75–100 %). For microbiological outcomes of these infections, the end of therapy response was 80–100 % and the test of cure response was 88–100 %.
-
-
-
Impact of the introduction of a 13-valent pneumococcal vaccine on pneumococcal serotypes in non-invasive isolates from 2007 to 2016 at a teaching hospital in Japan
More LessPurpose. To prevent severe invasive pneumococcal infection, pneumococcal conjugate vaccines (PCVs) were introduced in Japan in 2010, and in 2013 a pneumococcal 13-valent conjugate vaccine (PCV13) was included in the routine vaccination schedule for infants. In this study, we analysed the antimicrobial susceptibilities and capsular types of pneumococci isolated from non-invasive patient sites from 2007 to 2016 to assess the impact of the introduction of PCV13.
Methodology. A total of 618 pneumococcal isolates collected at a teaching hospital from 2007 to 2016 were used. These isolates were characterized by capsular typing, multilocus sequence typing and antimicrobial susceptibility testing.
Results. Capsular typing indicated that, after the introduction of the PCV, the proportion of PCV13 serotypes decreased (P<0.01), while non-PCV13 serotypes became diverse. In particular, increases in 22 F, 15A and 23A were noted among non-PCV13 serotypes. Regarding antimicrobial susceptibility, the non-susceptibility rate to penicillin of pneumococci that showed higher minimum inhibitory concentrations (MICs) than the susceptibility breakpoint decreased, and pneumococci tended to become susceptible. However, all type 23A pneumococci and 77.8 % of type 15A pneumococci showed the reverse trend, with low susceptibility to penicillin. Furthermore, all 15A and 23A isolates had macrolide resistance genes.
Conclusion. These data suggest that PCVs can prevent infections caused by PCV serotypes. However, since non-PCV13-type pneumococci, in particular 15A and 23A, which have acquired multidrug resistance, have already emerged over time, the development of a novel vaccine targeting a broader spectrum of pneumococci is warranted.
-
- Disease, Diagnosis and Diagnostics
-
-
-
Serum C-reactive protein relationship in high- versus low-virulence pathogens in the diagnosis of periprosthetic joint infection
More LessLittle is known about the relationship between the virulence of pathogens in periprosthetic joint infection (PJI) and C-reactive protein (CRP) levels. In this context, we assessed the performance of CRP for PJI. We collected the following data from 987 cases of total joint revision due to PJI and 386 cases of aseptic revision: age, gender, comorbidities, values for serum CRP, leukocytes, microbiology for preoperatively taken aspirations and at least 2 intraoperative biopsies, and presence or absence of a draining sinus. The mean CRP value in the PJI group was 50.2 mg l−1 (sd=62.2), while a lower CRP value of 11.6 mg l−1 (sd=25.3) was found in the control group. There were no significant differences for the CRP values between patients with and without draining sinus (P=0.4423). The difference in CRP between high-virulence and low-virulence micro-organisms was significant for both the hip and the knee (P<0.0001). For the hip, the area under the receiver operating characteristic curve (AUC) of CRP as a diagnostic marker for PJI was 0.830 and, for the knee, the AUC was 0.884. The optimal cutoff point for CRP as a diagnostic marker of PJI, calculated using Youden’s index, was 8.90 mg l−1 for the hip and 9.99 mg l−1 for the knee. The study results add valuable new information regarding the organism profile that may help with the diagnostic workup and with the research and development of new strategies for diagnosing and treating PJI.
-
-
- Medical Mycology
-
-
-
Molecular epidemiology of otomycosis in Isfahan revealed a large diversity in causative agents
More LessPurpose. To elucidate the clinical and microbial epidemiology of otomycosis in Isfahan, Iran.
Methodology. From January 2016 to January 2017 all patients clinically suspected of otomycosis at Al-Zahra Hospital, Isfahan, Iran were recruited. Specimens were taken using sterile swabs by an otorhinolaryngologist and subjected to culture and microscopy using potassium hydroxide and Giemsa stain. Isolated fungi were identified based on morphological and molecular characteristics.
Results. Otomycosis was confirmed in 97/120 patients (80.8 %). Females (72.2 %) and patients aged 30–39 years (33 %) were more commonly affected than others. Manipulation of ear canal (62.9 %) was the most common predisposing factor. Pruritus was observed in 84.54 % of the patients followed by hearing impairment (81.4 %), and most episodes were detected over the summer (50.5 %). Culture was positive for 81 (83.5 %) of confirmed cases and molds were the most prevalent causative agents (n=51, 63 %) followed by yeasts (n=19, 23.4 %) and yeast/mold mixes (n=11, 13.6 %). For the 16 remaining patients, no growth was seen in culture despite a positive result on direct examination. In total, 92 isolates (63 molds and 29 yeasts) were recovered in culture. Application of molecular methods showed 18 fungal species and the vast majority of them belonged to Aspergillus (n=53, 57.6 %) and Candida genus. Among the species involved, Candida parapsilosis (n=22, 22.7 %) and Aspergillus tubingensis (n=15, 15.5 %) were the most encountered species.
Conclusion. Outcomes from this study showed a different picture of prevalence, where C. parapsilosis and A. tubingensis but not Aspergillus niger were the most species encountered from patients suffering from otomycosis.
-
-
-
-
Serum IgE and IgG reactivity to Aspergillus recombinant antigens in patients with cystic fibrosis
More LessPurpose. The diagnosis of aspergillosis in cystic fibrosis (CF) patients remains a challenge due to overlapping features of both diseases. This is further complicated by inconsistent antibody reactivity to the currently used crude antigen, which has led a more focused evaluation of the efficacy of IgE response to a number of pure Aspergillus fumigatus recombinant proteins in patients with CF and asthma. In this study, we dissected the IgE and IgG responses to multiple A. fumigatus recombinant antigens in CF patients with different Aspergillus diseases.
Methodology. Serum IgE and IgG antibodies were measured in 12 CF patients with allergic bronchopulmonary aspergillosis (ABPA), 12 with Aspergillus sensitization (AS) and 12 with Aspergillus bronchitis (AB) against recombinant antigens Asp f1, f2, f3, f4 and f6.
Results. The ABPA group showed significantly greater IgE reactivity to Asp f1, f2, f3 and f4 compared to patients with AS. Patients with AB expressed higher IgG positivity to Asp f1 and Asp f2 compared with those with ABPA. There were very low IgE antibody levels against all recombinant antigens in patients with AS. Aspf1 IgG reactivity in ABPA patients correlated with positive culture.
Conclusion. The use of multiple recombinant antigens may improve the diagnostic accuracy in CF complicated with ABPA or AB. Asp f1 reactivity may relate to the presence of actively growing Aspergillus spp., which might be a useful marker for guiding antifungal therapy in ABPA.
-
- Molecular and Microbial Epidemiology
-
-
-
The epidemiology of Shiga toxin-producing Escherichia coli infections in the South East of England: November 2013–March 2017 and significance for clinical and public health
More LessPurpose. This study describes the epidemiology of Shiga toxin-producing Escherichia coli (STEC) infections in a population in the South East of England.
Methods. From 1 November 2013 to 31 March 2017 participating diagnostic laboratories reported Shiga toxin gene (stx) positive real-time PCR results to local public health teams. Stx positive faecal samples/isolates were referred to the Gastrointestinal Bacteria Reference Unit (GBRU) for confirmation by culture and typing by whole genome sequencing (WGS). Key clinical information was collected by public health teams.
Results/Key findings. Altogether, 548 faecal specimens (420 were non-travel associated) were stx positive locally, 535 were submitted to the GBRU. STEC were isolated from 42 %, confirmed by stx PCR in 21 % and 37 % were PCR negative. The most common non-travel associated STEC serogroups were O157, O26, O146 and O91. The annualized incidence of confirmed STEC infections (PCR or culture) was 5.8 per 100 000. The ratio of O157 to non-O157 STEC serogroups was 1:7. The annualized incidence of non-O157 haemolytic uraemic syndrome-associated Escherichia coli (HUSEC) strains was 0.4 per 100 000. Bloody diarrhoea was reported by 58 % of cases infected with E. coli O157, 33 % of cases infected with non-O157 HUSEC strains and 12 % of other lower risk non-O157 strains. Overall, 76 % of non-O157 HUSEC isolates possessed the eae virulence gene.
Conclusions. HUSEC including serogroup O157 were uncommon and more likely to cause bloody diarrhoea than other STEC. The routine use of stx PCR testing can influence clinical management. Understanding the local epidemiology facilitates a proportionate public health response to STEC, based on clinical and microbiological characteristics including stx subtype(s).
-
-
- Pathogenesis, Virulence and Host Response
-
-
-
Diversity of strategies used by atypical enteropathogenic Escherichia coli to induce attaching and effacing lesion in epithelial cells
More LessPurpose. This study aimed to characterize 82 atypical enteropathogenic Escherichia coli (aEPEC) isolates, obtained from patients with diarrhea in Brazil, regarding their adherence patterns on HeLa cells and attaching and effacing (AE) lesion pathways.
Methodology. The adherence and fluorescence-actin staining (FAS) assays were performed using HeLa cells. AE lesion pathways were determined through the detection of tyrosine residue 474 (Y474) phosphorylation in the Tir protein, after its translocation to host cells, and by PCR assays for tir genotyping and detection of Tir-cytoskeleton coupling protein (tccP) genes.
Results. Regarding the adherence pattern, determined in the presence of d-mannose, 12 isolates (14.6 %) showed the localized adherence (LA)-like pattern, 3 (3.7 %) the aggregative adherence pattern and 4 (4.9 %) a hybrid LA/diffuse adherence pattern. In addition, 36 (43.9 %) isolates displayed an undefined adherence, and 26 (31.7 %) were non-adherent (NA), while one (1.2 %) caused cell detachment. Among the 26 NA aEPEC isolates, 11 showed a type 1 pilus-dependent adherence in assays performed without d-mannose, while 15 remained NA. Forty-eight (58.5 %) aEPEC were able to trigger F-actin accumulation underneath adherent bacteria (FAS-positive), which is an important feature of AE lesions. The majority (58.3 %) of these used the Tir-Nck pathway, while 39.6 % may use both Tir-Nck and Tir-TccP pathways to induce AE lesions.
Conclusion. Our results reveal the diversity of strategies used by aEPEC isolates to interact with and damage epithelial host cells, thereby causing diarrheal diseases.
-
-
-
-
Sequence similarity searches for morphine biosynthesis enzymes in bacteria yield putative targets for understanding associations between infection and opiate administration
More LessExploiting the immunosuppressive, analgesic and highly addictive properties of morphine could increase the success of a bacterial pathogen. Therefore, we performed sequence similarity searches for two morphine biosynthesis demethylases in bacteria. For thebaine 6-O-demethylase and codeine O-demethylase, we found strong alignments to three ( Pseudomonas aeruginosa , Klebsiella pneumoniae and Acinetobacter baumannii ) of the six ESKAPE pathogens ( Enterococcus faecalis , Staphylococcus aureus , K. pneumoniae , A. baumannii , P. aeruginosa and Enterobacter species) that are commonly associated with drug resistance and nosocomial infections. Expression of the aligned sequence found in P. aeruginosa (NP_252880.1/PA4191) is upregulated in isolates obtained from cystic fibrosis patients. Our findings provide putative mechanistic targets for understanding the role of morphine in pathogenicity.
-
- Prevention, Therapy and Therapeutics
-
-
-
Fast-acting bactericidal activity of olanexidine gluconate against qacA/B-positive methicillin-resistant Staphylococcus aureus
More LessThe qacA/B gene is one of the major determinants of resistance to antiseptics in methicillin-resistant Staphylococcus aureus (MRSA). Here, we compared the fast-acting bactericidal activity of skin antiseptics, including olanexidine gluconate (OLG), a new biguanide antiseptic agent introduced in Japan, against clinical qacA/B-positive MRSA strains by determination of minimum bactericidal concentration and time–kill assay. Our findings provide, for the first time, data indicating that the fast-acting bactericidal activity of OLG against qacA/B-positive MRSA is higher than that of chlorhexidine gluconate, even though both are biguanide antiseptics.
-
-
-
-
Antimicrobial peptides prevent bacterial biofilm formation on the surface of polymethylmethacrylate bone cement
More LessPurpose. Antibiotic-loaded polymethylmethacrylate-based bone cement has been implemented in orthopaedics to cope with implant-related infections associated with the formation of bacterial biofilms. In the context of emerging bacterial resistance to current antibiotics, we examined the efficacy of short antimicrobial peptide-loaded bone cement in inhibiting bacterial adhesion and consequent biofilm formation on its surface.
Methodology. The ability of α-helical antimicrobial peptides composed of 12 amino acid residues to prevent bacterial biofilm [methicillin-resistant Staphylococcus aureus (MRSA), Staphylococcus epidermidis , Pseudomonas aeruginosa and Escherichia coli ] formation on the surface of model implants made from polymethylmethacrylate-based bone cement was evaluated by colony-forming unit (c.f.u.) counting of bacteria released by sonication from the biofilms formed on their surfaces. The biofilms on model implant surfaces were also visualized by light microscopy after staining with tetrazolium dye (MTT) and by scanning electron microscopy.
Results. When incorporated in the implants, these peptides caused a mean reduction in the number of bacterial cells attached to implants’ surfaces (by five orders of magnitude), and 88 % of these implants showed no bacterial adhesion after being exposed to growth media containing various bacteria.
Conclusion. The results showed that the antibiofilm activity of these peptides was comparable to that of the antibiotics, but the peptides exhibited broader specificity than the antibiotics. Given the rapid development of antibiotic resistance, antimicrobial peptides show promise as a substitute for antibiotics for loading into bone cements.
-
Volumes and issues
-
Volume 73 (2024)
-
Volume 72 (2023 - 2024)
-
Volume 71 (2022)
-
Volume 70 (2021)
-
Volume 69 (2020)
-
Volume 68 (2019)
-
Volume 67 (2018)
-
Volume 66 (2017)
-
Volume 65 (2016)
-
Volume 64 (2015)
-
Volume 63 (2014)
-
Volume 62 (2013)
-
Volume 61 (2012)
-
Volume 60 (2011)
-
Volume 59 (2010)
-
Volume 58 (2009)
-
Volume 57 (2008)
-
Volume 56 (2007)
-
Volume 55 (2006)
-
Volume 54 (2005)
-
Volume 53 (2004)
-
Volume 52 (2003)
-
Volume 51 (2002)
-
Volume 50 (2001)
-
Volume 49 (2000)
-
Volume 48 (1999)
-
Volume 47 (1998)
-
Volume 46 (1997)
-
Volume 45 (1996)
-
Volume 44 (1996)
-
Volume 43 (1995)
-
Volume 42 (1995)
-
Volume 41 (1994)
-
Volume 40 (1994)
-
Volume 39 (1993)
-
Volume 38 (1993)
-
Volume 37 (1992)
-
Volume 36 (1992)
-
Volume 35 (1991)
-
Volume 34 (1991)
-
Volume 33 (1990)
-
Volume 32 (1990)
-
Volume 31 (1990)
-
Volume 30 (1989)
-
Volume 29 (1989)
-
Volume 28 (1989)
-
Volume 27 (1988)
-
Volume 26 (1988)
-
Volume 25 (1988)
-
Volume 24 (1987)
-
Volume 23 (1987)
-
Volume 22 (1986)
-
Volume 21 (1986)
-
Volume 20 (1985)
-
Volume 19 (1985)
-
Volume 18 (1984)
-
Volume 17 (1984)
-
Volume 16 (1983)
-
Volume 15 (1982)
-
Volume 14 (1981)
-
Volume 13 (1980)
-
Volume 12 (1979)
-
Volume 11 (1978)
-
Volume 10 (1977)
-
Volume 9 (1976)
-
Volume 8 (1975)
-
Volume 7 (1974)
-
Volume 6 (1973)
-
Volume 5 (1972)
-
Volume 4 (1971)
-
Volume 3 (1970)
-
Volume 2 (1969)
-
Volume 1 (1968)
Most Read This Month