-
Volume 65,
Issue 10,
2016
-
Volume 65,
Issue 10,
2016
Volume 65, Issue 10, 2016
- Prevention and Therapy
-
-
-
Intracellular, biofilm-inhibitory and membrane-damaging activities of nimbolide isolated from Azadirachta indica A. Juss (Meliaceae) against meticillin-resistant Staphylococcus aureus
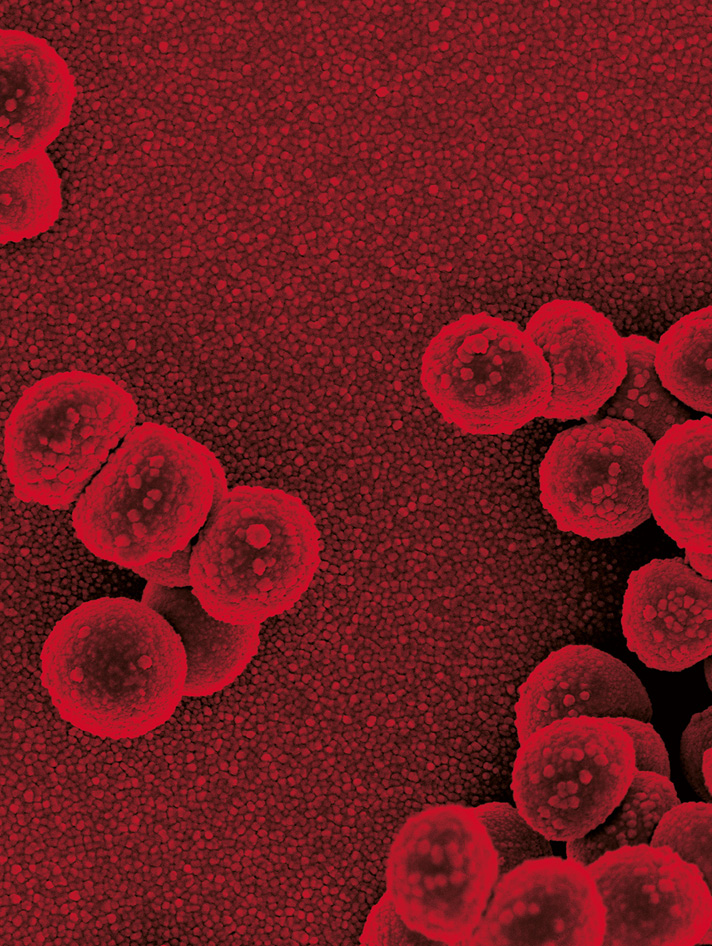
More LessStaphylococcus aureus is a leading aetiologic agent of nosocomial- and community-acquired infectious diseases worldwide. The public health concern regarding staphylococcal infections is inflated by the increasing occurrence of multidrug-resistant strains, e.g. multidrug- and meticillin-resistant S. aureus (MDR MRSA). This study was designed to evaluate the intracellular killing, membrane-damaging and biofilm-inhibitory activities of nimbolide isolated from Azadirachta indica against MDR MRSA. I n vitro antibacterial activity of nimbolide was determined by performing MIC, minimal bactericidal concentration (MBC) and time-kill kinetic studies. Bacterial membrane-damaging activity was determined by membrane perturbation and scanning electron microscopy (SEM) examination. Biofilm-inhibitory activities were determined by SEM. Cellular drug accumulation and assessments of intracellular activities were performed using Vero cell culture. SEM revealed that nimbolide caused significant membrane damage and lysis of the S. aureus cells. The biofilm structure was disrupted, and the biofilm formation was greatly reduced in the presence of nimbolide as examined by SEM. The level of accumulation of nimbolide in Vero cells incubated for 24 h is relatively higher than that of ciprofloxacin and nalidixic acid (C c/C e for nimbolide > ciprofloxacin and nalidixic acid). The viable number of intracellular S. aureus was decreased [reduction of ~2 log10 c.f.u. (mg Vero cell protein)−1] in a time-dependent manner in the presence of nimbolide (4× MBC) that was comparable to that of tetracycline and nalidixic acid. The significant intracellular, biofilm-inhibitory and bacterial membrane-damaging activities of nimbolide demonstrated here suggested that it has potential as an effective antibacterial agent for the treatment of severe infections caused by MDR MRSA.
-
-
-
-
In vitro activities of tedizolid compared with other antibiotics against Gram-positive pathogens associated with hospital-acquired pneumonia, skin and soft tissue infection and bloodstream infection collected from 26 hospitals in China
More LessShuguang Li, Yu Guo, Chunjiang Zhao, Hongbin Chen, Bijie Hu, Yunzhuo Chu, Zhijie Zhang, Yunjian Hu, Zhiyong Liu, Yan Du, Qiaodi Gui, Ping Ji, Ji Zeng, Bin Cao, Quan Fu, Rong Zhang, Zhongxin Wang, Chao Zhuo, Xianju Feng, Wei Jia, Yan Jin, Xuesong Xu, Kang Liao, Yuxing Ni, Yunsong Yu, Xiuli Xu, Zhidong Hu, Jin-E Lei, Qing Yang and Hui WangTo evaluate the in vitro antimicrobial activities of tedizolid, linezolid and other comparators against clinically significant Gram-positive cocci isolates from hospital-acquired pneumonia (HAP), skin and soft tissue infection (SSTI) and bloodstream infection (BSI), 2140 nonduplicate isolates (23.7 % isolated from HAP, 46.8 % from SSTI and 29.5 % from BSI) were consecutively collected in 26 hospitals in 17 cities across China during 2014. These pathogens included 632 methicillin-resistant Staphylococcus aureus, 867 methicillin-sensitive Staphylococcus aureus, 299 coagulase-negative Staphylococcus (CoNS), 104 Enterococcus faecalis, 99 Enterococcus faecium, 13 Streptococcus pneumoniae, 23 α-haemolytic Streptococcus and 103 β-haemolytic Streptococcus. MICs of routine clinical antibiotics were determined by broth microdilution method according to the Clinical and Laboratory Standards Institute guidelines 2015. Tedizolid, linezolid, vancomycin, daptomycin, teicoplanin and tigecycline showed high in vitro activity against Gram-positive pathogens (≥98.0 % susceptible), and tedizolid exhibited four- to eight fold greater activity than linezolid against the pathogens tested, with MIC90s of methicillin-resistant Staphylococcus aureus, α-haemolytic Streptococcus and β-haemolytic Streptococcus (0.25 vs 2 µg ml−1); methicillin-sensitive Staphylococcu s aureus, E. faecalis and E. faecium (0.5 vs 2 µg ml−1); methicillin-resistant CoNS and methicillin-sensitive CoNS (0.25 vs 1 µg ml−1); and Streptococcus pneumoniae (0.125 vs 0.5 µg ml−1). Tedizolid MIC90s associated with different infections did not show significant differences, and the drug exhibited excellent activity against surveyed Gram-positive pathogens associated with HAP, SSTI and BSI, including linezolid-nonsusceptible strains. These data suggest that tedizolid could be an alternative to linezolid for the treatment of infections caused by Gram-positive organisms.
-
- Correspondence
Volumes and issues
-
Volume 73 (2024)
-
Volume 72 (2023 - 2024)
-
Volume 71 (2022)
-
Volume 70 (2021)
-
Volume 69 (2020)
-
Volume 68 (2019)
-
Volume 67 (2018)
-
Volume 66 (2017)
-
Volume 65 (2016)
-
Volume 64 (2015)
-
Volume 63 (2014)
-
Volume 62 (2013)
-
Volume 61 (2012)
-
Volume 60 (2011)
-
Volume 59 (2010)
-
Volume 58 (2009)
-
Volume 57 (2008)
-
Volume 56 (2007)
-
Volume 55 (2006)
-
Volume 54 (2005)
-
Volume 53 (2004)
-
Volume 52 (2003)
-
Volume 51 (2002)
-
Volume 50 (2001)
-
Volume 49 (2000)
-
Volume 48 (1999)
-
Volume 47 (1998)
-
Volume 46 (1997)
-
Volume 45 (1996)
-
Volume 44 (1996)
-
Volume 43 (1995)
-
Volume 42 (1995)
-
Volume 41 (1994)
-
Volume 40 (1994)
-
Volume 39 (1993)
-
Volume 38 (1993)
-
Volume 37 (1992)
-
Volume 36 (1992)
-
Volume 35 (1991)
-
Volume 34 (1991)
-
Volume 33 (1990)
-
Volume 32 (1990)
-
Volume 31 (1990)
-
Volume 30 (1989)
-
Volume 29 (1989)
-
Volume 28 (1989)
-
Volume 27 (1988)
-
Volume 26 (1988)
-
Volume 25 (1988)
-
Volume 24 (1987)
-
Volume 23 (1987)
-
Volume 22 (1986)
-
Volume 21 (1986)
-
Volume 20 (1985)
-
Volume 19 (1985)
-
Volume 18 (1984)
-
Volume 17 (1984)
-
Volume 16 (1983)
-
Volume 15 (1982)
-
Volume 14 (1981)
-
Volume 13 (1980)
-
Volume 12 (1979)
-
Volume 11 (1978)
-
Volume 10 (1977)
-
Volume 9 (1976)
-
Volume 8 (1975)
-
Volume 7 (1974)
-
Volume 6 (1973)
-
Volume 5 (1972)
-
Volume 4 (1971)
-
Volume 3 (1970)
-
Volume 2 (1969)
-
Volume 1 (1968)
Most Read This Month